Back to disabilitydenials.com
If you become disabled and can no longer work, disability insurance plans and government disability programs offer potential sources of replacement income in the form of disability benefit payments.
These sources of income can become a lifeline for you and your family should the unthinkable happen.
The Complete Guide to Disability Claims, Insurance and Benefits is your one-stop source for disability benefit information. Our easy-to-read guide explains:
- who is eligible for disability benefits
- what type of benefits are available to you
- how to apply for disability benefits
- how to make sure your disability claim is properly prepared
- tips that make the difference between claim approval and claim denial
- what to expect during the disability claims handling process
- how to handle difficult situations that may arise
- what to expect once benefits are granted
- why benefits are denied or terminated, and what to do about it
What type of disability claim do you have?
The following benefits may be available to you:
- Short Term Disability (STD) Insurance and Long Term Disability (LTD) Insurance – These are disability insurance plans sold and administered by insurance companies. You may have purchased a long-term or short-term insurance policy through an insurance agent. Or, your employer may sponsor a group disability plan that covers you and other employees.
- Social Security Disability Insurance (SSDI) – SSDI insures disabled workers who have paid into the system through FICA taxes. It is a Federal disability insurance program managed by the Social Security Administration (SSA).
- Supplemental Security Income (SSI) – Also provided by the Social Security Administration, SSI benefits are available to elderly, blind, and disabled people with little or no income or assets.
- Veterans Disability Compensation – A tax-free financial benefit paid to Veterans with disabilities who became sick or injured as a result of active military service (both combat and non-combat related), and for some post-service disabilities. Veterans’ disability benefits are managed by the Department of Veterans Affairs (VA).
Get Started with Your Disability Claim
To learn about your benefits, click on a link below for information that will help you get started with your claim.
- Guide to Short Term Disability (STD) Insurance Claims
- Guide to Long Term Disability (LTD) Insurance Claims
- Guide to Social Security Disability Insurance (SSDI) / Supplemental Security Income (SSI)
- Guide to Veterans Disability Compensation Claims
Disclaimer: The information in this guide is solely informational; it is not intended to add to or replace any advice given by an attorney or qualified non-attorney representative who is familiar with your specific circumstances.
Table of Contents: Short Term Disability
Guide to Short Term Disability (STD) Insurance Claims
Chapter 1: About Short Term Disability Insurance
- Short Term Disability (STD) & Long Term Disability (LTD) Policies Are Often Connected
- Waiting Periods
- A Short Term Disability Claim Will Always Be an “Own Occupation” Claim
- Your STD Claim Will Not Be Offset by Social Security Disability Benefits
Chapter 2: The Initial Application for STD Benefits
Chapter 3: If Your STD Claim Is Denied: Do Not Give Up
Chapter 4: Getting Legal Representation
Chapter 5: Short Term Disability Insurance vs. Family Medical Leave Act (FMLA)
Guide to Short Term Disability (STD) Insurance Claims
Chapter 1: About Short Term Disability Insurance
The purpose of short term disability insurance is to financially protect yourself for a limited period of time while you are unable to work due to illness or injury. STD partially replaces your income until you either return to work or go on long-term disability.
- Employers may purchase short term disability coverage to offer to employees under a group disability benefit plan. Sometimes employees may also contribute to their short term disability premiums.
- Some STD plans are paid for and administered by the employer (and not by an insurance company.)
- You may also purchase short term disability insurance privately from an agent or broker.
The length of the typical STD claim is from 90 days (3 months) to 180 days (6 months). Other policies cover as little as one week and up to 24 months.
STD can pay up to 100 percent of your base salary.
Short Term Disability (STD) & Long Term Disability (LTD) Policies Are Often Connected.
Does your insurance policy cover both STD and LTD? It is important that you know. Read through your entire policy and understand how it is set up.
If you are covered by a plan that offers short term and long term disability coverage, make sure you know how they coordinate. Many insurance plans are structured so that a claim for short term disability insurance is the required first step to filing a long term disability claim.
And although you may have both STD and LTD coverage in your policy, they are separate plans, each covering a separate period of time.
For example, you may have a 3-6 month Short Term Disability policy for which you would submit an application to receive benefits. Suppose, after the STD coverage is used up, your “short term” disability worsens or evolves into a long term disability. You must reapply for the Long Term Disability portion of the plan.
When this is the case, it is critical that you have a clearly defined record of the disability’s onset.
Waiting Periods
Both short term disability and long term disability plans have a waiting period—also called an elimination period or a qualifying period—that must be met before you are eligible for benefits. This is the time span between disability onset and the point at which coverage becomes payable.
STD waiting periods are measured in days, where LTD waiting periods can be months—the time will be specified in your policy. Ideally, the STD policy matches the length of the LTD waiting period to avoid a lapse in coverage.
A Short Term Disability Claim Will Always Be an “Own Occupation” Claim
STD policies are written to award financial benefits if your disability leaves you unable to do the substantial duties of your own occupation. In other words, you are disabled from performing your usual job tasks (as opposed to just any task.)
For example, if you work in construction and your disability limits your ability to hammer or climb a ladder, you would likely be awarded STD benefits under the policy.
The distinction between “own occupation” and “any occupation” becomes very critical in the event you need to apply for long term disability benefits, after your short term benefits are exhausted.
Read more about Own Occupation vs. Any Occupation in a long term disability claim.
Your STD Claim Will Not Be Offset by Social Security Disability Benefits
The Social Security Disability Insurance (SSDI) program pays benefits only for long term and permanent disabilities. Since your short term disability claim will generally last no more than 3-6 months, those benefits will not be offset by SSDI payments. SSDI is not a short term solution for disability situations.
Learn about Social Security Disability offsets and how they can affect an award of long term disability benefits.
Chapter 2: The Initial Application for STD Benefits
Group Disability Claim: If your coverage is under a group plan through your employer, request the claim forms from your Human Resources department.
Private Disability Claim: If coverage is under your own private plan, also referred to as an Individual Disability Insurance (IDI) plan, contact your insurance provider for the disability claim forms.
Filing the Short Term Disability Claim
The Application Process
Each insurance provider will have its own specific claim submission information that you must follow—whether a claim is filled out and submitted online, by mail on specific forms, or over the telephone.
The claims filing process is basically the same for both short term and long term disability claims, and in many policies the STD claim is just the prerequisite first step to filing the LTD claim.
For detailed information about the filing process, please see:
The Initial Application: How to File a Long Term Disability Claim
What to expect on the claim forms:
Generally the paperwork includes (but is not limited to):
- Claimant’s Statement
- Employer’s Statement
- Attending Physician’s Statement (also referred to as a Physician’s Statement of Disability, or Physician’s Certificate for Disability Benefits)
- Authorization to Obtain and Disclose Information
You will need to have your doctor complete the insurance company’s Attending Physicians Statement form. In addition, the insurance adjuster will need all medical records and supporting documentation pertaining to your condition. Also to be sent is the list of all medical providers who treat you for the disability.
Do not rely on the insurance provider to gather your medical records. It is your responsibility to assemble and forward all medical and vocational evidence to support your claim of disability to the insurer. This includes medical records, doctors’ opinions and evaluations, functional capacity evaluations and other important materials to prove you are unable to work.
The insurance company will review your information and investigate your case to make a determination resulting in the approval, denial, or request for additional information.
If your claim is approved, you will receive benefit payments from the insurance company, a third party administrator, or your employer, depending on the insurance plan arrangement.
If your claim is denied, you will generally be notified in writing.
Tips for a Successful Application
Claimants rarely expect the countless difficulties that emerge as they submit their claims and wait for their benefits. Many initial claims are challenged or denied by the insurers.
It is important to take every possible action to ensure your case is rock-solid and well-founded. The following link will ensure you leave nothing to chance:
20 Tips to Help You Win Benefits on Your Initial Application
Chapter 3: If Your STD Claim Is Denied: Do Not Give Up
As a whole, initial claims for short term disability benefits are more likely to be approved than those for long-term disability insurance. Still, STD claim denials are not uncommon.
STD claims that evolve into LTD claims become much more expensive for the insurer to pay out. Valid claims for short term disability benefits are sometimes denied—or benefits are discontinued—in order for insurance providers to avoid extensive long-term payments.
By denying short term benefits, the insurer effectively reduces your eligibility for long term benefits, paving the way for LTD claim denial.
If your short term disability claim is denied, do not give up or think the process is over. Insurance policies must allow you the opportunity to appeal, or contest, an unfavorable decision.
File an Appeal
While the appeals process is more or less the same across insurance companies, each insurer and policy will have its own unique procedures and timelines. And because policy language rules, you need to review the wording in your policy – plus the information sent in your denial letter – to understand what your responsibilities are for filing an appeal properly and timely.
The time in which you have to file an appeal can be as short as 45 to 60 days, sometimes longer, depending on the policy.
An appeal is much more than filling out more paperwork. The letter of denial will include the reason the insurer denied the claim. Your appeal should be based largely upon the reason your claim was denied.
On appeal, you need to supplement your case with further supporting medical evidence, physician’s opinions, medical expert testimony, as well as corroborative statements from co-workers, family and friends regarding their observations of your disabling condition.
If the information and forms you need to appeal are not sent to you with the denial letter, contact the insurance provider to request they immediately send the necessary information to you.
While you can file an appeal on your own, enlisting the help of a disability insurance lawyer can greatly improve your chances of a getting a fair award of benefits.
Chapter 4: Getting Legal Representation
Initially, claimants are not skeptical of the insurance industry or the disability insurance process. Once their claim is denied, they are at a loss about what to do to get their badly needed insurance coverage.
When it comes to filing a successful appeal, experienced legal counsel is in order. A disability insurance lawyer can take the burden of proof off your shoulders, develop your case properly and apply the law to your benefit, and provide all of the necessary evidence to effectively appeal a wrongly denied insurance claim.
Learn more about getting legal assistance.
Chapter 5: Short Term Disability Insurance vs. Family Medical Leave Act (FMLA)
Both STD and Family Medical Leave are in place to help you if you become disabled and cannot work for a temporary time span. However, they are very different sources with different purposes. It is important not to confuse the two.
Family Medical Leave Protects Your Job
FMLA does not compensate for lost wages. If is a federal program that prevents employers from firing employees who miss weeks or months of work, because they are injured or very sick.
You may be eligible for up to 12 workweeks of leave per year under FMLA. The leave is unpaid: your employer is not required by law to pay you for missed time.
FMLA rules apply in all 50 states, and generally affect companies with 50 or more employees. FMLA also helps you be away from work due to a family member’s medical emergencies, and for maternity leave and adoption.
Short Term Disability Insurance Replaces Income
STD is a disability insurance plan that is totally financial in nature. It does not affect job security; i.e., your employer is not required to hold your job. The insurance carrier that provides the coverage promises to pay on a legitimate disability claim, per policy limits. STD generally starts after any paid sick days are used up, and other policy conditions are met.
Whether purchased privately or provided by an employer, STD coverage is optional. STD only covers the named insured on the policy, and no other family members.
FMLA and STD often work together. Visit the Department of Labor website to learn if you qualify for FMLA.
Table of Contents: Long Term Disability
Guide to Long Term Disability (LTD) Insurance Claims
Chapter 1: About Long Term Disability Insurance
Chapter 2: Types of Disability Insurance Policies
Chapter 3: Group Disability Claims Are Regulated by Federal ERISA Law
Chapter 4: Individual Disability Claims (Non-ERISA) Are Regulated by State Insurance Law
Filing a Claim:
Chapter 5: The Initial Application: How to File a Long Term Disability Claim
Chapter 6: 20 Tips to Help You Win Disability Benefits on Your Initial Application
Chapter 7: How Will Your Long Term Disability Benefits Be Paid?
Chapter 8: Is Your LTD Policy Subject to Exclusions and Limitations?
Chapter 9: What You Must Prove to Win Your Disability Insurance Claim
Chapter 10: RFC – Developing Your Residual Functional Capacity to Prove your Claim
Chapter 11: Why You Need to Appoint Your Own SSD Attorney Representative
Chapter 12: Attorney Representation in a Disability Claim
If Your Claim Is Denied:
Chapter 13: Disability Claim Denied? File an Administrative Appeal
Chapter 14: Legal Representation for Administrative Appeals
Chapter 15: Insurer’s Tactics and Claim Denial
If Your Administrative Appeal Is Denied:
Chapter 16: File an ERISA Lawsuit
Chapter 17: File a Lawsuit on an Individual (Non-ERISA) Disability Insurance Claim
Chapter 18: Legal Representation during Your Lawsuit
Chapter 19: How Does an Attorney Get Paid?
Chapter 20: Getting Legal Representation: What to Look For
Guide to Long-Term Disability (LTD) Insurance Claims
Chapter 1: About Long Term Disability Insurance
The onset of disability can rob you of your ability to work and make a living. Disability insurance policies protect employees and working individuals from the loss of income in the event they become disabled due to illness, injury or other serious impairment.
Insurance companies provide various forms of disability coverage ranging from group workplace benefits to customized, individual benefits, each with varying definitions of “disability” and levels of coverage.
Examples of some of the largest companies that provide disability insurance include Hartford Life, Unum, CIGNA, MetLife, The Standard, Lincoln Financial, Prudential, Aetna, Dearborn National, Liberty Mutual, Provident Life and Paul Revere Insurance.
Chapter 2: Types of Disability Insurance Policies
Disability policies are separated into two main forms regarding duration of coverage: Short Term and Long Term disability coverage.
Policies are also classified into two main types regarding which laws regulate the policy. These two types include group (employer-based) plans and individual (personal) disability policies.
As explained below, the laws governing each are quite different, and will affect your claim in a big way.
Short Term Disability (STD)
Short Term Disability insurance helps replace lost wages if a disability keeps you out of work for a limited time. STD claims are often the prerequisite first step in the long term disability insurance claims process. Short term policies typically cover from 80 to 100% of your salary.
For more information visit our Guide to Short Term Disability claims.
Long Term Disability (LTD)
The purpose of long term disability insurance is to replace a portion of your income when you are unable to work for an extended period of time, or permanently, due to a severely disabling condition or impairment.
LTD policies typically cover about 60–65% of your salary. The cost of long-term disability insurance varies between group plans offered by employers and individual plans, which tend to be more expensive.
Most long term disability policies have a waiting, or qualifying period. This means that before you can apply for LTD benefits, you first must
- apply for and receive all of the short term disability benefits available under the insurance carrier’s policy, or
- satisfy a waiting period by being disabled for up to six months.
LTD benefits are generally paid for 24 months if you become unable to work at your own job. This is referred to as the Own Occupation period.
After the 24-month “own occupation” period, you can potentially receive LTD benefits until age 65, if you continue to prove that you are disabled from doing any job in light of your age, education and training available to you in your area. This becomes the Any Occupation period and, as explained further in this guide, is harder to prove.
Group Disability Plans (Provided by Your Employer)
Long term disability insurance may be sponsored by or offered through your workplace as part of a group disability plan. The laws that govern most group policies are federal laws known by the acronym “ERISA” – The Employee Retirement Income Security Act.
When you file a group disability claim and ERISA laws take over, your claim is suddenly subjected to very strict, complicated federal laws. If your claim is denied, you must follow rigid legal procedures and obey strict deadlines as you appeal your case.
Individual Disability Insurance Plans (Buying Coverage on Your Own)
Coverage purchased on your own behalf is referred to as individual disability insurance (IDI) or privately purchased disability insurance. Many professionals in specialty or high-end occupations such as doctors, dentists, lawyers, CEOs and others buy IDI as a form of income replacement should they become disabled by illness or injury.
Individual coverage is underwritten for you specifically. It is not part of an employer’s group insurance plan. However, individual policies are sometimes used to supplement an employee’s group disability policy.
Individual policies are regulated under state insurance laws regarding bad faith and contract law. These laws are designed to protect the insured and beneficiaries from unfair practices by insurers.
Insurance Riders and Occupation-Specific Policies
A rider is a provision for optional benefits added to the basic policy at additional cost. Individual disability insurance policies are often customized with specific features and supplemented by riders.
By drafting very individualized and occupation-specific policies, a person is able to protect the income level that he or she has worked to achieve over many years. Of course this increases the premiums considerably.
For example,
- Own-Occupation: occupation-specific coverage that states the definition of disability is your specific occupation or sub-specialty rather than the broader definition of “other occupation” or “any occupation.” Example: your occupation is defined as “orthopedic surgeon” instead of “practicing medicine.”
- No limitations or exclusions of coverage concerning disabilities due to mental disorders
- Portability – Your policy travels with you from one job to the next.
- Partial disability benefit riders allow benefits under certain conditions if you are unable to do some or all of the duties of your own occupation full time.
- Cost of living riders allow for increased benefits due to inflation
- Lifetime extension riders allow options for lifetime benefits beyond a certain age
- A Residual Disability Rider will pay if you cannot return to work full time. It can also pay in the event your income is not completely restored. For example, you are a dentist and you go back to work on a full time basis. However, your dental practice has endured financial hardship because of your absence. Residual disability payments (a percentage of the full disability benefit) would help cover this loss as it is a result of your disability.
As you can see, there is a big difference between group and individual plans. If you are denied long term disability benefits under either type of plan, you have the right to appeal the denial.
The remedies that are available to you as a claimant appealing a denied a group policy claim are very different than if your claim is under an individual policy.
The next section explains these differences in detail, so you can better prepare for all communications and dealings with the insurance provider.
Chapter 3: Group Disability Claims Are Regulated by Federal ERISA Law
What Is ERISA?
ERISA stands for the Employee Retirement Income Security Act of 1974. It is a federal law that controls the management of Employee Benefit Plans and the compensation and remedies of the beneficiaries of these Plans.
Practically all long-term disability plans offered by a private employer are governed by ERISA.
If you are challenging a denied disability claim under an ERISA governed plan or policy, you must adhere to ERISA regulations and procedures. That means you must appeal the denial to the same insurance company that denied the claim.
Since ERISA claims are based on federal law, the law and procedures are generally the same in all 50 states. All state law remedies are preempted, meaning they do not apply to an ERISA claim.
ERISA Does Not Apply to Privately Purchased Insurance
If you bought individual or family disability coverage on your own (not through an employer) then ERISA does not apply. Privately purchased disability coverage falls under state contract and insurance laws.
h3 id=”h-other-disability-plans-not-covered-by-erisa”>Other Disability Plans Not Covered by ERISA
- Government employees: Government plans are excluded from ERISA coverage. This generally includes federal, state and local governments including school districts and public universities.
- Church Plans: Employees of qualifying religious institutions such as a church, synagogue or mosque are generally exempt from ERISA.
- Self-Employed Individuals: Self-employed individuals are not governed by ERISA if only the individual and their family are covered.
- Some Partnerships: Similarly, partners in a partnership with a plan that only covers partners, but no employees is not an ERISA governed plan.
- Pass Through Plans: Voluntary Plans where the employer contributed nothing to the plan and merely acted as a “pass-through” are exempted from ERISA if all requirements are met. These are extremely rare as the LTD carriers generally require employer contributions to set up the plan for the express purpose of receiving ERISA protection.
Protections You Lose under ERISA Laws
The following explains what protections you lose under most group disability plans, in the case of a claim denial or dispute.
- ERISA Offers No State Protections: You cannot sue for:
- Emotional distress
- Consequential (or special) damages
- Loss of credit claims
- Prejudgment interest for breach of contract
- Tortious interference with contract
- Statutory insurance violation claims
- Deceptive trade acts or unfair practices
- Bad faith
- Punitive damages
- Mandatory attorney fee reimbursement
- Your Remedies Are Severely Limited Under ERISA. If the insurer unfairly denies your claim, you can only sue for what the insurer should have paid you in the first place. That means the most the insurer will have to pay is the original claim amount and nothing else. With no penalty to deter an insurance company from wrongly denying a valid claim, many claims under group plans are denied.
- No Right to Jury Trial: A jury will not decide your claim. Group disability insurance carriers know they don’t have to worry that a jury of your peers will hold them accountable.
- No Treating Physician Rule: ERISA laws allow the insurance carrier to disregard your treating doctor’s opinions and rely on their own doctor’s opinions if they so choose.
- Little Government Regulation: ERISA law offers little direction as to how an insurance policy should be written. This leaves disability insurance underwriters free to write the policy as they wish. Thus many provisions and clauses are not favorable to the claimant. Often the only incentive to offer favorable provisions is competition from other disability insurance providers.
- You Must Prove the Insurer “Abused Its Discretion”: In a disability insurance claim brought under state law, you only have to prove it is “more likely than not” that you are disabled. Not so for claims brought under ERISA. There, the burden is on you to prove that the insurer “Abused Its Discretion” by denying your claim. You must prove that the insurer had “No Reasonable Basis” for its decision. Insurance companies will rely on their own “independent” exam or review by their own doctors and experts — in order to have some evidence to show that its decision was reasonable.
Chapter 4: Individual Disability Claims (Non-ERISA) Are Regulated by State Insurance Law
Private LTD policies are contracts between you and the insurance provider. Claim disputes under these policies are governed by state contract and bad faith law. If an insurer denies your claim, you can appeal the decision. However, these appeals are often nothing more than an internal review with the same insurer that initially denied the claim.
When an acceptable settlement with an insurance company cannot be reached, bad faith insurance claim litigation becomes necessary. Litigation of private policies are held in state or federal court. The burden of proof is the same as a civil trial. You are allowed a jury trial, and may fully engage in evidence and discovery.
State Protections Available
Depending on the state, the protections and damages that are available to you in a dispute over a private disability claim include:
- Emotional distress
- Consequential (or special) damages
- Loss of credit claims
- Prejudgment interest for breach of contract
- Tortious interference with contract
- Statutory insurance violation claims
- Deceptive trade acts or unfair practices
- Bad faith
- Punitive damages
- Mandatory attorney fee reimbursement
Filing a Claim:
Chapter 5: The Initial Application: How to File a Long Term Disability Claim
Caution: A Successful Claim Requires Building a Strong Case
The initial application process for long term disability benefits may seem as simple as filling out the forms sent by your insurer. Yet this is never the case.
A great amount of preparation and forethought is required on the claimant’s end to prepare a claim that does not end up delayed or denied.
There are many pieces of evidence you will need to collect, complete and submit. Numerous bits of information must be carefully worded and supported to build an ironclad case.
The remainder of this guide is designed to inform disability claimants how to put together and present a strong claim of disability to their insurance provider.
A qualified attorney can be a true asset in properly submitting a disability claim. He or she will work with your doctors and various medical experts to produce essential evidence, as well as anticipate the tactics insurers may resort to in efforts to deny paying a claim.
Consider consulting an attorney who has reviewed or appealed hundreds of LTD claims. A good lawyer will develop your case so that it is strong enough to prevent a denial based on allegations that you are not disabled under the terms of the policy, or for insufficient or partial information.
Learn more about getting legal assistance.
The Application Process
For both STD and LTD claims, all insurance companies have their standard packet of forms to be completed, but that is where the similarity ends. Each company’s paperwork is uniquely worded in critical ways.
For a group / ERISA policy, claim forms and filing information will be available to the claimant from the Human Resources department of the employer.
For a privately purchased policy, claim forms and filing information will be available to the policyholder directly from the insurance provider.
Your insurer will have submission information that you must follow—whether a claim is filled out and submitted online, by mail on specific paper copy forms, by fax or over the telephone.
What can you expect on the claim forms? Generally the paperwork includes (but is not limited to):
- Claimant’s Statement – You complete this form with your personal information, employment information, information about your claimed disability, your care and treatment (including a complete listing and contact information for all doctors, pharmacies and hospitals who treat you for the disability), other sources of income and benefits you have received or are receiving, and tax withholding information.
- Employer’s Statement (for group claims) – Your employer completes this form with information about the employer, about you as an employee, about your job, your insurability, withholding and reporting taxes, your pension plan, physical aspects of your job, last day worked, your reason for leaving work, job accommodation or return-to-work policies and salary.
- Attending Physician’s Statement – Medical information to be completed by your treating doctor should include the details of diagnosis, treatment, level of functional impairment (physical and psychiatric), and return to work expectation. Your doctor is requested to attach and send all medical records and supporting documentation relevant to your impairment.
- Authorization to Obtain and Disclose Information – This form grants the Insurance Company permission to obtain any information about you from any medical, pharmacy, business, insurance, financial, governmental or other organization or person with knowledge of you or your health.
You compile and review all of the above forms, statements and records, and submit them to the insurance company to review.
The Review Process
Do not assume the insurer help you gather your medical records from the providers. It is your responsibility to see that all medical and vocational evidence is collected and delivered to support your claim of disability to the insurer. This includes medical records, doctors’ opinions and evaluations, functional capacity exams and other relevant information to show you are unable to work.
The insurer will review and investigate your case and reach a decision to approve, deny or request more information.
NOTE: Claimants rarely expect difficulties to emerge as they submit their claims and wait for their benefits. The reality is, many initial claims are wrongfully challenged or denied by the insurers.
If your claim is approved, you will receive benefit payments from the insurance company or a third party administrator, depending on the insurance plan arrangement.
If your claim is denied, you will generally be notified in writing. You have the right to appeal the denial.
Go here for details on appealing a denied LTD claim.
It is important to take every possible action to ensure your case is rock-solid and well-founded. The following tips will ensure you leave nothing to chance; these tips are further explained throughout this guide.
Chapter 6: 20 Tips to Help You Win Disability Benefits on Your Initial Application
The following steps will help ensure that you do not leave anything to chance when filling out and submitting your initial application for a short term or long term disability claim.
1. Read Your Policy!
Read through your policy to know how your benefits are structured. If you do not have a copy, ask your employer or the insurance company for a copy. The exact terms and language in your disability policy is unique to you, and that language is what governs how benefits may be awarded or denied. Know the type of policy you have. Know how your policy defines “disability.”
2. Review the Claim Form.
Become familiar with the information you need to provide the insurance company before filling out the form.
The claim form will generally have:
- Employee or Claimant Statement
- Employer’s Statement (for group claims)
- Attending Physician’s Statement (also called a Physician’s Statement of Disability, or Physician’s Certificate for Disability Benefits)
- Authorization to Obtain and Disclose Information
Read and become familiar with all sections to know exactly what is expected of you, your employer and your physician. The claim forms typically do not allow room for the level of detail that a well-developed claim needs to present. Use additional paper so you can be as thorough as possible to explain the particulars of every aspect of your claim to the insurance adjuster.
There will be critical time limits you must follow. Make sure to read and understand the deadlines and cutoff dates required by the disability policy and the claim form.
3. Understand the Connection between Your STD and LTD Policies
Check to see whether your disability plan is set up where the short term and long term policies interact. Most long term policies often require that you exhaust all short term benefits in order to meet the elimination (waiting) period that is required before long term disability benefits will be paid.
For instance, your policy might have a 3-6 month short term disability policy for which you must initially submit an application. Once this STD coverage is exhausted, you would need to reapply for the long term disability portion of the plan. Denial of a short term claim will prevent the approval of a long term disability claim.
4. Understand your policy’s structure.
The initial term of most LTD plans, usually 24 months, is referred to as the “Own Occupation” portion of the plan. After that 24-month term has expired, to continue benefits you must meet the tougher “Any Occupation” definition of disability to continue to receive benefits. You need to develop a case with evidence that will stand up to this shifting definition of disability.
Know if your policy allows you to age out of coverage. Most policies naturally terminate at the claimant’s retirement age, either age 65 or the full Social Security Retirement Age for the individual claimant.
5. Know what medical conditions may be excluded or limited.
Check your policy to learn of any impairments that may have limited benefits. If is common for disability policies to restrict or exclude benefit payments for certain disorders.
For example, does your policy have limitations for
- impairments based on self-reported symptoms such as chronic fatigue
- soft tissue injuries not supported by objective medical evidence
- Pre-existing conditions
- Mental or psychological disorders
You can increase your chances of receiving a favorable decision by concentrating on medical conditions and functional limitations that are not subject to limitations, exclusions or preexisting limitation exclusions written into your policy.
6. Talk with Your Doctor about Your Decision to Apply for Disability Benefits.
Your doctor is your ally. Review your medical records with him or her. As the claimant, the burden is on you to submit to the insurance company sufficient medical evidence that you are too impaired to continue working at your current job.
This should include
- comprehensive medical documentation of your diagnosed condition
- your doctors’ assessment of your functional limitations resulting from your disability
- meeting all required deadlines
Reach agreement with your doctor about presenting your case in the best possible way. Prepare your doctor for the likelihood of being interviewed by the insurance company, and receiving follow-up forms from the insurer.
7. Alert Your Doctors to Expect Phone Calls from Insurance Company Doctors.
Help prepare your doctors for the demands the insurance company is about to make. These requests may include asking your doctor to complete and submit monthly disability forms. One missed form can lead to claim denial. The insurer will also call your doctor to discuss your case directly. Explain to your doctor that he or she needs to take that call.
8. Assume you are under surveillance.
Insurance companies often use covert video surveillance to catch you doing something that you stated in your claim you are disabled from doing. Surveillance might include recording your drives to doctor’s appointments or the grocery store. Insurers may also be watching social media activity. Also, insurers may send their claims investigators to your home without warning to question you about your claim while you are off guard. You have the right to refuse a surprise visit and ask them to reschedule for a more acceptable time for you.
9. Be Ready for Unusual and Difficult Requests by the Insurer
The process of filing a claim and securing disability benefits might be more challenging than expected. One such challenge is that insurers often ask for documents or forms to be filled out and submitted repeatedly. Be prepared and proactive: keep up with and complete relentless requests for the same information.
10. Prepare to file for Social Security Disability Insurance.
Your LTD insurer will require you to file for Social Security Disability benefits within 12 months of disability. The reason is because the insurance provider is allowed to offset (subtract the amount) of your Social Security Disability benefits from the benefits they owe you. You do need to file for SSDI, but be aware if your insurer wants you to use their recommended SSDI representative.
11. Know How Your Disability Policy Defines Your Salary vs. Bonus.
Most policies base monthly benefits on your base salary and leave out bonuses or commissions. But every policy is different. Find out if your policy factors in other forms of compensation such as bonuses and commissions and how these forms of compensation and your salary are defined and calculated.
12. Pick your onset of disability date.
You will need to state the date that you became disabled. Your date of disability can affect your claim a couple of ways: (1) if there is a question of a preexisting exclusion, or other certain limitations and exclusions in the policy; (2) the onset of disability date must be alleged to be during a period where insurance coverage is in effect.
If it is possible to time your claim for disability, it is best to have an experienced attorney look at these issues before you make your disability claim.
13. Compare Your Job Description to Your Employer’s Description of Your Job
The first 24 months of LTD benefits will be based on an “own occupation” definition of disability. So it is important that your job description captures what you really do.
Write down what your actual job entails. Include your physical, mental and travel requirements—job duties that you perform routinely. Examine your description in contrast to your employer’s version of what you do.
Do the two match? It is vital to the success of your short term or long term disability claim that your physician’s description of your functional limitations clearly demonstrates—when viewed alongside your true job description— that you can no longer do that job.
14. Work on a Draft Copy of the Application – Then Make a Final Copy
Make some copies of the blank application form, and prepare a working copy that you can edit and perfect. Then make a final version on the original claim form that is neat, clean and presents a well-founded, justified claim for disability. Make and keep at least one copy of your final version.
15. Do Not Use Absolute Statements to Describe Your Limitations
When describing your physical limitations, do not use absolutes like “always” and “never.” Statements such as “I can never stand for 30 minutes” or “I always need a walker to get from my bed to the chair” are often easily contradicted by the insurance company. Less definite words like “frequently, sometimes, occasionally or seldom” are less apt to be challenged.
Once an absolute statement is disproved, whether by your own medical documentation or by video surveillance, you are labeled a fraud and the insurance company will have grounds for denial.
16. Watch Out for Unclear or Evasive Questions or Choices in the Application
Some disability insurance applications ask questions that wrongly assume facts that are not true, or offer multiple choice answers that only lead to an unfair conclusion.
For example, a claim form may ask what level of activity you are capable of. You have the following choices: heavy, medium, light or sedentary. The result is that any answer you choose can result in your claim being denied. A fair question would also include the choice “none of the above.”
17. Know the Difference between Total and Partial Disability
Most policies will provide definitions of Total and Partial disability and the requirements of both.
There can be a big difference between total vs. partial disability in terms of collecting disability payments. Partial disability sometimes results in a lower payment because the person may still be able to work, but cannot do the same types of tasks as before.
If you think you may be able to work part time and plan on filing for partial disability, take a close look at the mathematical formulas and limits.
18. Keep a Record of all Medical Providers and Prescriptions.
In the application, include an up-to-date list of your medical providers with verified contact information. If your physicians cannot be reached through the information submitted in the application, they may be treated as if they don’t exist.
Also specify all prescription medications and the side effects of each medication.
19. Follow All Filing and Appeal Deadlines Precisely
You must file your application for disability within specific time periods stated in your policy.
If your short term disability claim is denied, you have a very short timeframe in which to appeal—often as little as 45 days depending on the policy.
If your long term disability claim is denied or your existing benefits are terminated, you typically have 180 days to appeal the denial.
If your appeal is denied, you have a limited amount of time to file your lawsuit that can vary from state to state or could be limited under the terms of the policy.
20. Consult with experienced disability insurance attorneys.
It is wise to consult with an attorney who concentrates in disability insurance law and ERISA law prior to filing your application. It is essential to consult with one before appealing a denied claim.
Chapter 7: How Will Your Long Term Disability Benefits Be Paid?
A Percentage of Your Salary
Most disability policies pay 60% of a claimant’s salary. If you work on a commission or other non-salaried basis, the insurer uses a calculation described in your policy to arrive at a benefit amount.
- Benefits Are Usually Paid Up to Retirement Age: If you can continue to prove ongoing disability, benefits are often paid through age 65, depending on the policy.
- Special Rules if Disability Occurs After Age 60: If your disability begins after age 60, benefits are paid according to a schedule in the policy. Depending on your age, benefits will be paid for a maximum number of months. For example, a claimant who becomes disabled at age 63 would get 36 months; age 64, 30 months.
Partial or Residual Disability Benefit
Some policies allow you to work on a part time basis or carry out lighter job duties if you are disabled from functioning at your full-time level of work. A partial or residual disability benefit is payable if your disability causes your income to drop more than a certain percentage—typically 20% below your regular income.
Your policy will require you to make a certain percentage less than your regular salary. Normally in this case, you would be earning less money than if you worked full time or full duty.
How Social Security Disability Benefits Can Offset LTD Payments
Most policies have a Social Security offset. This means if you get a monthly Social Security Disability (SSD) benefit, the amount of the SSD check is “subtracted” from the monthly LTD check.
For example, you have been getting monthly checks for $2,500 from your long term disability insurance company. Now you start receiving monthly SSD checks in the amount of $1,000. Your insurance provider will reduce their LTD payment from $2,500 to $1,500. You still receive a total of $2,500 a month, but $1,000 from SSD and $1,500 from LTD.
Retroactive SSDI benefits can be deducted from your LTD benefits, meaning you must pay the retroactive award amount back to the insurance provider.
Watch Out for Overpayments
Like most claimants, you might file a claim for Social Security Disability benefits around the same time as you apply for long term disability benefits.
As part of the LTD insurance application, you may notice a form that you must sign telling the insurance company how you will “pay back” the SSD offset. You can choose to have the insurance company estimate how much your SSD benefit will be. The insurer will then “deduct” that estimate from your monthly LTD benefit.
However, most claimants do not take this option. Instead they choose the lump sum option. This pays back the SSD offset in one lump sum to the insurance company, so the claimant can receive their full LTD monthly benefit.
But this option often works against the claimant. For many disabled workers, the SSD backpay can be a substantial sum of money. Figure in that it can take up to two years for a claimant to receive an SSD award. In this case your SSD back benefits can amount to thousands of dollars.
Once you receive the SSD award and back benefits, the insurance company will act to recover the full amount of back benefits. But consider that you have been disabled from working, getting just 60% of your former wages. The reality is that most claimants have already spent their SSD back benefits to pay bills.
If you are unable to pay back the full SSD amount in a lump sum to the insurance company, the company can hold back the entire LTD monthly benefit towards the amount of Social Security Disability offsets that your “owe.”
This problem is made worse when the SSD award arrives just as you reach the “any occupation” definition of disability at 24 months, because the insurance company may cut off benefits when the policy changes, leaving you with a large overpayment to repay.
Read more about the “Any Occupation” definition of disability.
Other Possible Offsets (Deductions)
Offsets may also occur with other types of income, such as worker’s compensation benefits, certain retirement benefits, settlements from lawsuits, and state-provided short term disability benefits.
Sometimes the total of all offsets is greater than the monthly LTD benefit amount. In this case, most policies provide for a minimum monthly payment of $100 or 10% of the monthly LTD benefit.
Chapter 8: Is Your LTD Policy Subject to Exclusions and Limitations?
Make sure your policy covers your condition! No policy covers every condition, and those diseases, injuries and impairments that are not covered, or have limited coverage, may carry great weight regarding your claim’s success.
Get familiar with your policy’s exclusions and limitations. If the language is unclear, ask the insurance company. We describe common examples below; but read your policy carefully to know exactly what you can expect.
Disabilities Caused by Preexisting Conditions
A pre-existing condition is an illness or injury that began or occurred before you were covered under the policy. Most policies “exclude” pre-existing conditions, which means you cannot receive benefits if those illnesses or injuries occurred in the past.
Pre-existing exclusions usually come into effect when a person has been eligible for benefits for less than a year (sometimes this period is two years.) Besides the preexisting condition exclusion time period of a year, there is also a “look back” period, usually the three months prior. This means if you were treated for the claimed condition during the three-months before the effective date of your policy, you are ineligible for benefits.
Basically, if you apply for LTD benefits less than a year after you sign up for the benefit, the insurer will review all your medical and pharmacy records for the entire year plus the look back period, looking for a pre-existing condition.
Pre-existing exclusions are typically very broad. For example, you may have been prescribed a medication for the treatment of anxiety during the look back period. Later, you develop a back problem with muscle spasms, and file a disability claim for that condition.
The same medication that was prescribed to treat your anxiety is now being prescribed to treat muscle spasms. The insurance adjuster will access your pharmacy records and see that you took this medication in the past. The adjuster may stretch the “pre-existing’ interpretation of your claim record and say that you are being treated for muscle spasms because were prescribed this medication in the past. This enables the insurer to deny disability benefits based on the preexisting condition exclusion.
Mental or Nervous Condition Limitation
Most policies have a 24 month mental health limitation. This means that benefits for mental health conditions such as depression, anxiety or bipolar disorder will only be paid for 24 months. This is a common reason for benefits to initially be awarded but cut-off after two years.
Depression as a Secondary Condition
In cases of chronic pain, it is not uncommon for claimants to develop depression as a secondary condition. The insurance adjuster may try to classify depression as a mental impairment, so that benefits will be paid for only 24 months. The adjuster may also try to classify a cognitive problem or side effects from narcotic pain medications as a mental impairment.
Make sure the insurance carrier does not misrepresent your physical disability as mental.
Limited Coverage of Self-Reported Symptoms
LTD policies can limit benefits if certain criteria are not met. Many diseases and injuries can be convincingly demonstrated through “objective medical evidence.” Objective evidence usually refers to diagnostic tests like MRIs, blood work or X-rays.
Many claimants struggle with disabling conditions that cannot be based on such telltale, obvious proof. These conditions are primarily based on self-reported symptoms, as opposed to objective medical evidence.
Some symptoms, like chronic pain, some diseases, like fibromyalgia and chronic fatigue syndrome, and some injuries like soft tissue injuries—do not show up on any “objective” tests. These symptoms and diseases are diagnosed by the doctor based on a history of clinical consultation and observation, patient reports, medical history, exclusionary testing, treatment and prognosis.
h3 id=”h-non-exertional-limitations”>Non-Exertional Limitations
Non-exertional limitations are also mostly self-reported and therefore, mostly disregarded by the insurance provider. Examples of non-exertional limitations include fatigue, headache, intellectual and cognitive limitations (such as concentrating, anxiety, depression), memory loss and medication side effects.
Chapter 9: What You Must Prove to Win Your Disability Insurance Claim
h3 id=”h-your-policy-s-definition-of-disability”>Your Policy’s Definition of Disability
There is no one legal definition of disability. The definition varies among insurance companies and between policies. Definitions applied by the insurance industry differ from the Social Security Administration’s definition and the Dept. of Veterans Affairs’ definition of disability.
You must read your policy to know what the definition of disability is that you must meet. Usually it is roughly similar to, “due to sickness or injury the employee is unable to perform the material and substantial duties of his or her own occupation.”
After 24 months pass, the definition in most LTD policies shifts from “own occupation” to “any occupation,” which is more rigid – meaning you must prove you cannot perform any job for which you are reasonably qualified based on your education, training, or experience.
Not only does the insurance company define disability; the insurer also interprets the terms in their definition and decides whether you are disabled or not. This creates an inherent financial conflict of interest.
h3 id=”h-your-treating-doctor-s-opinion-vs-the-insurance-company-s-in-house-opinion”>Your Treating Doctor’s Opinion vs. the Insurance Company’s In-House Opinion
To determine if you are disabled, the insurance provider relies on their own employees or consultants to review your medical records. The opinions of these in-house nurses or doctors are often different than your own treating doctor’s opinion. Thus the insurer may take the stance that your doctor’s opinion is not supported by the medical records.
In reviewing this type of activity, the Supreme Court has decided that the “treating physician rule” (as used by the Social Security Administration) does not apply in LTD insurance determinations.
According to the treating physician rule, in SSDI claims if your treating doctor says you are disabled, that opinion is given “great weight” towards the decision.
In private and group LTD plans however, the Supreme Court has ruled that your doctor’s opinion that you are disabled should be taken into account as “a factor” in the insurer’s decision to award disability benefits.
h3 id=”h-an-award-of-social-security-disability-does-not-influence-your-insurer-s-decision”>An Award of Social Security Disability Does Not Influence Your Insurer’s Decision
For someone under 50 years old, Social Security’s definition of disability states that he or she must be unable to work at any occupation available in the national economy. This actually is a stiffer requirement than an LTD definition.
And since Social Security has somewhat different standards for disability, the insurance company will ignore an award of benefits by Social Security by stating that the rules are different.
h3 id=”h-but-the-insurance-company-helped-me-get-social-security-disability”>But the Insurance Company Helped Me Get Social Security Disability
If you are approved for LTD benefits, your insurer will help you apply for and receive Social Security Disability benefits. You should know that your award of SSDI benefits helps the insurer financially.
Insurance carriers contract with another company that represents claimants before the SSA. Your insurer will reduce your LTD monthly benefit by the amount Social Security Disability pays you, and will require you to “pay back” the back benefits received from Social Security.
h3 id=”h-proving-the-economics-of-a-long-term-disability-claim”>Proving the Economics of a Long Term Disability Claim
The insurance industry uses various measures to control the cost of paying on individual disability insurance claims, or to award or deny valid claims.
One strategy used to deny claims filed by medical professionals (under their private policy) is to classify a doctor or dentist’s past work as a generalist, rather than a specialist. These practices are largely based on surgical procedures such as endoscopies, eye laser treatments, routine dental surgery or skin biopsies.
For example, an ophthalmologist suffers neurological problems affecting hand dexterity and can no longer perform eye surgery. Suddenly forced to work as a general eye doctor in an office setting, by no means will he or she make the same kind of income as when he or she regularly performed eye surgery.
By classifying a specialist’s past work as a generalist, the insurer protects its profits without taking into account any loss of income for the disabled medical specialist. This is an important tactic to watch out for, and a valid component to demonstrate and prove on your claim for benefits.
h3 id=”h-the-vocational-review-by-the-insurer”>The Vocational Review by the Insurer
If the insurance adjuster finds you to be “not disabled,” he or she may perform what is called a “vocational review.” Using any restrictions the insurance adjuster says that you have, and with the skills derived from your past work history, a vocational analyst will produce a list of jobs that you can perform.
The vocational analyst will state that these occupations are available in your home region and that the job will pay usually, at least 60-80% of your pre-disability earnings. These reviews are often flawed and make unreasonable suggestions for occupations.
h3 id=”h-your-residual-functional-capacity-rfc”>Your Residual Functional Capacity (RFC)
Your RFC – residual functional capacity – is based on the physical level of work you are able to perform as an impaired person. The Dictionary of Occupational Titles and Social Security define work as:
- sedentary
- light
- medium
- heavy
- very heavy
A sedentary job is comparable to an office setting or clerical work: Sitting for up to six hours a day, standing or walking up to two hours a day and lifting and carrying up to 10 pounds, like files or small objects.
A light job requires that you are able to stand or walk up to six hours per day and frequently lift and carry 10 pounds and occasionally lift and carry 20 pounds. Most medical and dental professions and specialties are considered light jobs. Other examples of light job classification might be a cashier or security guard.
A medium job, like a nurse or commercial truck driver, requires the ability to lift 50 pounds;
Heavy work, like construction, requires the ability to lift 100 pounds; and
Very heavy work requires the ability to lift more than 100 pounds.
Proving what your RFC currently is and what may be expected from you in the future can be a critical factor in your disability claim. The following section of this guide will help you better understand your RFC and how to apply it to support your case.
Chapter 10: RFC – Developing Your Residual Functional Capacity to Prove your Claim
Being disabled means you suffer from an impairment and symptoms which result in physical and/or mental limitations. Your RFC is the most you can do despite your limitations.
RFC helps to assess the maximum remaining ability you have to do sustained work tasks in an ordinary job setting on a regular and continuing basis. A regular and continuing basis means work done for eight hours a day, for five days a week, or an equivalent schedule.
Your RFC is expressed in terms of the exertional classifications of work. As mentioned above, these classifications are described as sedentary, light, medium, heavy, or very heavy work.
h3 id=”h-exertional-activities-for-ltd-claims”>Exertional Activities for LTD Claims
Your RFC must be understood in terms of the seven primary strength, or exertional, activities of work. These consist of three work positions and four worker movements of objects, as follows:
Three work positions:
- Sitting
- Standing
- Walking
Four worker movements of objects:
- Lifting
- Carrying
- Pushing
- Pulling
h3 id=”h-definition-of-residual-functional-capacity”>Definition of Residual Functional Capacity
To determine what you can still do regardless of your impairment, the insurance company’s claims analyst should consider all relevant medical and non-medical evidence.
This includes medical records, opinions and assessments by treating doctors, evaluations of the medical evidence by non-examining physicians, as well as your testimony and the testimony of others who have observed you.
h3 id=”h-the-five-rfc-levels”>The Five RFC Levels
Remember the five exertional RFC levels—sedentary, light, medium, heavy, and very heavy.
Each is defined in terms of the degree that the seven primary strength demands of jobs are required: sitting, standing, walking, lifting, carrying, pushing and pulling.
The extent that the seven primary strength demands are required are explained below:
SEDENTARY WORK
- Sitting should generally total approximately six hours of an 8-hour workday.
- Periods of standing or walking should generally total no more than 2 hours of an 8-hour workday.
- Lifting no more than 10 pounds at a time.
- Occasionally lifting or carrying articles like docket files, ledgers and small tools.
- The term “occasionally” means occurring from very little up to one-third of the time.
LIGHT WORK
- Requires standing or walking off and on, for a total of approximately six hours in an 8-hour workday.
- May involve sitting most of the time, but with some pushing and pulling of arm-hand or leg-foot controls which require greater exertion than in sedentary work.
- Lifting no more than 20 pounds at a time.
- Frequent lifting or carrying of objects weighing up to 10 pounds.
- The term “frequent” means occurring from one-third to two-thirds of the time.
- If someone can do light work, he or she also can do sedentary work, unless there are additional limiting factors such as loss of fine dexterity or inability to sit for long periods.
MEDIUM WORK
- Requires standing or walking off and on, for a total of approximately six hours in an 8-hour workday.
- As in light work, sitting may occur intermittently during the remaining time.
- Lifting no more than 50 pounds at a time.
- Frequent lifting or carrying of objects weighing up to 25 pounds.
- The term “frequent” means occurring from one-third to two-thirds of the time.
- If someone can do medium work, he or she also can do light and sedentary work.
HEAVY WORK
- Requires standing or walking off and on, for a total of approximately six hours in an 8-hour workday.
- Lifting objects weighing no more than 100 pounds at a time.
- Frequent lifting or carrying of objects weighing up to 50 pounds.
- If someone can do heavy work, he or she also can do medium, light, and sedentary work.
VERY HEAVY WORK
- Requires standing or walking off and on, for a total of approximately six hours in an 8-hour workday.
- Lifting objects weighing more than 100 pounds at a time.
- Frequent lifting or carrying of objects weighing 50 pounds or more.
- If someone can do very heavy work, SSA determines that he or she also can do heavy, medium, light, and sedentary work.
h3 id=”h-rfc-all-physical-and-mental-impairments-must-be-considered”>RFC: ALL Physical and Mental Impairments Must Be Considered
In evaluating your RFC, the claims examiner should consider all competent medical evidence, and after taking into account all of your impairments, assess the physical and mental activities that you can perform in a work setting.
The claims examiner must consider all symptoms, including pain.
h3 id=”h-rfc-effect-of-mental-impairments-must-be-considered”>RFC: Effect of Mental Impairments Must Be Considered
If you are claiming a mental disorder, the insurance company should determine whether this condition further limits the exertional tasks you are considered capable of doing.
The evaluation of RFC concerning mental disorders includes considering your ability to understand, to carry out and remember instructions and to respond appropriately to supervision, coworkers and customary work pressures in a work setting.
To properly make this assessment, evidence should include:
- History, findings, and observations from medical sources (including psychological test results) regarding the presence, frequency and intensity of hallucinations, delusions or paranoid tendencies; depression or elation; confusion or disorientation; conversion symptoms or phobias; psychophysiological symptoms; withdrawn or bizarre behavior; anxiety or tension.
- Reports of your activities of daily living and work activity, as well as testimony of third parties about your performance and behavior.
- Quality of daily activities, both in occupational and social spheres.
- Your ability to sustain activities, interests and relate to others over a period of time. The frequency, appropriateness and independence of the activities must also be considered.
- Your level of intellectual functioning.
- Your ability to function in a work-like situation.
h3 id=”h-rfc-non-medical-evidence-must-be-considered”>RFC: Non-Medical Evidence Must Be Considered
Non-medical evidence can play a key role in determining the functional limitations of a person suffering from a mental impairment.Suchsources include social workers and family members.
The courts have noted that ‘[i]nformation concerning an individual’s performance in any work setting (including sheltered work and volunteer or competitive work) … may be pertinent in assessing the individual’s ability to function in a competitive work environment.’
Determining RFC may also revolve around subjective reports of pain testified to by the claimant, in addition to and supporting medical facts, diagnoses and medical opinions based on such facts.
h3 id=”h-rfc-effect-of-absenteeism-on-the-ability-to-work-must-be-considered”>RFC: Effect of Absenteeism on the Ability to Work Must Be Considered
It is a good idea to have a vocational expert evaluate your impairment related to excessive absenteeism.
The insurance company should take into account (1) the fact that you would be absent from the workplace an excessive amount of time due to your condition, and (2) the treatment regimen required to treat your condition.
h3 id=”h-rfc-your-skill-level”>RFC: Your Skill Level
Skill levels are also defined by the Dictionary of Occupational Titles, based somewhat on how long it takes a person to learn a skill.
- Unskilled or semi-skilled jobs, rated at skill level 1, 2, or 3, take less than 30 days to learn;
- Skilled jobs are rated at 4, 5 and 6;
- Very skilled jobs are 7, 8 and 9.
h3 id=”h-rfc-own-occupation-standard-first-24-months”>RFC: “Own Occupation” Standard (First 24 Months)
The definition of “own occupation” is found in the insurance policy. Generally the definition is based on how the job is performed in the national economy as defined by the Dictionary of Occupational Titles—not how the claimant actually performs his or her own occupation.
For the first 24 months (or as defined in the policy) you only have to be unable to perform your “own occupation.”
Example A: Nursing falls in the Medium job class. Your occupation is a registered nurse, but because of a severe back impairment you are now restricted to lifting only 10 pounds; therefore, you would not be able to perform your own occupation.
Example B: You are a heart surgeon diagnosed with Parkinson’s disease. You are losing the ability to perform the essential tasks and duties of your own specialty practice. Cardiac surgery falls within the Light job class and is considered skilled work requiring years of training and education. Although you may still be able to lift 20 pounds and stand for 6 hours, tremors, weakness and the loss of fine dexterity must be taken into account as rendering you to be disabled from your own occupation.
h3 id=”h-rfc-any-occupation-standard”>RFC: “Any Occupation” Standard
After 24 months pass, the definition in most LTD policies shifts from “own occupation” to the broader definition of “any occupation.” Because the definition is broader, it is harder to prove. Now you must demonstrate that you cannot work in any job for which you are reasonably qualified based on your education, training, or experience.
h3 id=”h-rfc-salary-percentage-provision-under-any-occupation-standard”>RFC: Salary Percentage Provision under “Any Occupation” Standard
The “any occupation” standard usually includes a salary percentage requirement. This requirement is a provision in your policy stating that your insurance company cannot simply say that you qualify for any job, at any wage—and based on that, deny you disability benefits. Your insurer is obligated to find occupations that will pay you typically at least 80 percent of your pre-disability income.
Chapter 11: Why You Need to Appoint Your Own SSD Attorney Representative
Review your policy to see if it contains language requiring you to apply for Social Security Disability Insurance (SSDI). If it does, this provision also gives the insurance provider the right to offset (subtract) any Social Security benefits from the LTD monthly payment. Your LTD benefits will be reduced by the amount of Social Security disability that you receive.
For instance: If the insurance company is supposed to pay you $3,500 per month, and you also win Social Security Disability that pays you $1,800 per month, the LTD insurance company now only has to pay you $1,700 per month. You will also be required to reimburse the insurance company from the back benefits of any social security disability award.
h3 id=”h-the-insurer-s-motive-for-recommending-their-preferred-social-security-advocate”>The Insurer’s Motive for Recommending Their Preferred Social Security Advocate
The insurance company may urge that you allow their recommended SSDI representative to help you obtain Social Security disability benefits. They will frame this recommendation so that it appears they have your best interest in mind.
In reality, the insurer has a financial motive to help you win Social Security Disability benefits. By putting your SSDI case in the hands of their chosen claims management company, the insurance company can control who represents you before the Social Security Administration.
So the first thing your insurance company does is to solicit you to sign up with their recommended SSD representative to handle your SSD claim. Your insurance provider tells you they will pay the representative, making this is a free service to you. This tactic has you thinking that you are saving money and will be taken care of as far as receiving your SSD benefits.
Their purpose is to collect your back due benefits to reimburse your insurance company. This also gives the insurer a way to keep tabs on your SSDI claim, and rush in to take any back benefits you recover.
Remember, you may or may not actually owe these back benefits. Regardless of whether you owe it or not, this situation forms an obvious conflict of interest between you and the insurer’s recommended representative.
In most cases, representatives or advocates who get referrals from LTD providers are not attorneys, meaning
- you will not be protected by attorney-client privilege, and
- the representatives are not held to same level of ethical standards as attorneys.
That is the motivation for the LTD insurance company to persuade you to use their chosen SSD representative. These reps are working for the insurance company, not you. Their business is to facilitate the insurance company’s collection of overpayment.
The truth is, you are obligated to repay all back benefits to the insurance company anyway. Nothing is gained on your behalf, and money may be lost because you are not in control of what amount of back benefits are truly owed to the insurance company.
h3 id=”h-attorney-client-privilege”>Attorney-Client Privilege
Suppose the SSA denies your claim. The insurer then can use the non-attorney advocate’s disclosure that your SSD claim is denied as fuel for denying or terminating LTD benefits. Another conflict of interest.
LTD insurance carriers collaborate with non-attorney “advocates” or “representatives” because attorney-client privilege does not exist between you and the advocate. The advocate can tell everything they know about your case to the LTD carrier.
Conversely, a qualified, independent Social Security Disability attorney is bound by law to serve and protect your best interests 100% of the time. They will do all they can to ensure your claim is properly developed, that you are adequately prepared for hearings, and that your interests are protected.
h3 id=”h-a-non-attorney-advocate-cannot-represent-you-in-federal-court”>A Non-attorney Advocate Cannot Represent You in Federal Court
If your SSDI claim is denied during the administrative appeal, your last remaining remedy is to appeal your case to the federal courts. Non-lawyer representatives cannot argue denied SSDI claims to federal court on appeal. Their capabilities stop with answering questions concerning administrative policies and procedures.
Only an attorney can provide advice on the law. Even so, many general lawyers who do not specialize in Social Security Disability law are neither prepared nor willing to appeal Social Security disability claims to federal court. Aside from the skill and knowledge base, disability lawyers are prepared for the significant demand on time and resources.
h3 id=”h-attorney-accountability”>Attorney Accountability
Attorneys are bound by the ethical rules of the legal profession and are subject to the discipline of the courts and bar authorities. The rules of professional conduct obligate lawyers to ardently and competently represent their clients, charge only reasonable out-of-pocket costs, and maintain good communication with the client to keep them informed on the status of claim. A lawyer is never allowed to represent a client if the representation involves a concurrent conflict of interest.
If a lawyer were to mishandle your case or violate any rules of professional conduct, you can file a grievance with their state bar. Non-attorney advocates or representatives are not members of, nor regulated by, state bars and are not subject to the same disciplinary measures as attorneys.
Chapter 12: Attorney Representation in a Disability Claim
Every claimant is different and every case is unique. The following are just some of the ways an experienced attorney helps claimants prepare and file a disability insurance claim:
- Complete all insurance company forms correctly and without making unintentional statements that could weaken your claim;
- Review your LTD policy and advise you on its meaning, the law and your options;
- Obtain your complete claim file from the Insurance Company according to Federal ERISA statutes;
- Obtain medical reports and opinion evidence regarding your disability;
- Review your medical records and suggest additional testing to develop and prove your case;
- Fortify your claim file with further medical evidence and data;
- Consult with qualified Vocational Experts to get opinion evidence rebutting an insurance company’s denial;
- Obtain and develop evidence regarding your “Residual Functional Capacity” that is the key to your disability claim;
- Develop evidence to refute surveillance video;
- Develop evidence to refute the credibility of the insurance company’s doctors and vocational experts;
- Quickly and effectively file your administrative appeal when necessary;
- Correctly calculate your benefits;
- File a legal brief arguing the legal, medical and vocational issues in your case;
- File a lawsuit in Federal Court if necessary;
- Conduct discovery in the Federal Court case such as filing interrogatories and requests for production, as needed, as well as taking all necessary depositions;
- Respond to Motions for Summary Judgment and trying your lawsuit;
- Let the insurance company know that they cannot run over you.
If Your Claim Is Denied:
Chapter 13: Disability Claim Denied? File an Administrative Appeal.
After the claim is filed and evaluated, the insurance company will make a decision and either grant the claim or deny the claim. If the claim is granted, the insurance company will begin to pay monthly benefits. If the claim is denied, you should receive a “denial letter.”
h3 id=”h-the-letter-of-denial”>The Letter of Denial
The insurance company’s denial notice contains important information about your case, and how to appeal the decision. The letter will state:
- what evidence the insurance company reviewed when making its decision
- who reviewed the evidence—was it an in-house nurse case manager, a doctor hired as a consultant or only non-medical reviewers such as a Senior Claims Adjuster;
- the reasons your claim was denied and what medical evidence the claimant needs to prove disability;
- essential information regarding appeal procedures, including where to send the appeal and the time limits for filing the appeal.
h3 id=”h-time-limits-to-file-an-appeal”>Time Limits to File an Appeal
If the policy is a group benefit to employees (and thus governed by ERISA law) the appeal deadline is 180 days. Most non-ERISA (private) disability policies also give you 180 days to appeal.
In every case, it is very important to read the denial letter carefully, so no deadlines are missed. Under ERISA rules, you first have to “exhaust” or use up all available administrative appeals (usually one or two). Without that first step, you cannot file a lawsuit against the insurance company and your claim is over.
h3 id=”h-the-administrative-appeal-process”>The Administrative Appeal Process
ERISA Administrative Appeals vs Non-ERISA Administrative Appeals
While the laws and regulations are very different for ERISA vs. non-ERISA claims, the appeal process is basically the same for both ERISA and non-ERISA regulated claims.
Because ERISA regulations must be followed to the letter, and because so many claims fall under ERISA law, insurance companies tend to keep the same administrative appeals process and procedures in place for all claims.
The basic process is:
- You file a claim for disability,
- If the insurance carrier denies you, generally you have 180 days to respond,
- You go through an internal administrative appeals process,
- After that if you are still denied you have the right to file a lawsuit against the insurer.
The following explains in greater detail what anyone filing an ERISA claim should know about the administrative appeal process and the statute of limitations.
Under federal law, a claimant cannot bring a claim under judicial review until an internal review is carried out. This internal review, or administrative appeals procedure, begins when a claimant submits their proof of loss.
At that point, the Plan (i.e., the insurance company) has a set amount of time to carry out an internal review before the claim is taken to a judicial court. How does this work?
- The Plan has 45 days to make adverse benefit determination (i.e. to determine that benefits are not a medical necessity to the claimant or that the claimant is not eligible for benefits for any other reason).
- The Plan may use two 30 day extensions based on elements outside of their control, such as a claimant’s failure to submit documents necessary to make a decision based on their claim.
- The claimant must appeal a denial of their claim within 180 days of that denial.
The Plan has 45 days to resolve any appeal with one 45 day extension.
h3 id=”h-timeline-for-filing-a-lawsuit-the-statute-of-limitations”>Timeline for Filing a Lawsuit: The Statute of Limitations
The administrative appeal procedure alone can take up to a year or more.
If your initial claim was denied and then denied again on appeal, pay close attention to the timeline for filing a lawsuit, because the statute of limitations for civil actions in ERISA cases has recently changed.
Statute §502 (a)(1)(b) requires that you must exhaust the internal review process (and the insurer issues a final denial of your claim) before bringing your case to court for judicial review.
ERISA does not provide a statute of limitations for actions under §502 (a)(1)(b). However, your specific group disability plan may have a contractual limitation period that goes into effect as soon as you file your claim.
Most policies have a three year contractual statute of limitations period but many are as short as one year and some shorter than that.
h3 id=”h-mistakes-that-even-lawyers-make”>Mistakes That Even Lawyers Make
Even attorneys, if they are not experienced in disability issues, do not understand all of what must be proved in a disability claim. Many lawyers mistakenly believe that since your physician or the SSA has found you to be disabled, the insurance carrier must also find that you are disabled. Although these factors should be taken into account in your case, these two factors alone do not prove disability to the insurance company.
General practice attorneys may not comprehend the critical differences between “own occupation” and “any occupation,” or the subtle differences in each insurance plan’s definition of “disabled.” Inexperienced lawyers may argue the medical diagnosis, which does nothing to help prove disability.
In cases where a disabled individual is a physician, dentist or other highly skilled professional, one way an attorney must combat an insurance company’s denial tactics is by clearly proving the economics of their client’s case.
h3 id=”h-the-independent-medical-review”>The “Independent Medical Review”
Insurers often send the case record out for an Independent Medical Review. However, the label “independent” is a misnomer as this exam is by no means independent. Insurers team up with companies that employ doctors who perform these paper reviews.
The medical review companies advertise that they can help disability insurance carriers keep costs down. That is because these doctors seldom find a clamant disabled. Most of these doctors do not see patients anymore because they receive a large income from doing these file reviews.
h3 id=”h-the-independent-medical-exam-a-contractual-obligation”>The “Independent Medical Exam” – A Contractual Obligation
Often there is a contractual obligation stating that the insurance company will request to have you examined by an independent doctor.
Again, this type of exam is not truly “independent” when said doctor is working for the insurance company. Nonetheless, your disability policy is a contract and all contractual obligations must be followed. If you refuse to be examined, benefits can be terminated.
h3 id=”h-you-win-your-administrative-appeal-what-to-expect”>You Win Your Administrative Appeal: What to Expect
If you win the administrative appeal, you will receive back benefits (monthly benefits from the date benefits were cut-off) and be put “back on claim.” You will begin to receive monthly disability benefit payments.
You will still need to adhere to all contractual obligations and will need to continue to send in updated medical records and Attending Physician Statements to prove on-going disability.
Chapter 14: Legal Representation for Administrative Appeals
h3 id=”h-hiring-legal-counsel-to-help-with-administrative-appeal”>Hiring Legal Counsel to Help with Administrative Appeal
Some claimants try to appeal a denied long term disability claim on their own. A typical example is to prepare a one-paragraph or one-page appeal letter stating something similar to, “I appeal your decision. Please reconsider.”
If you have read through this disability guide, by now you know that this method is destined to fail. What matters most is the evidence and records you submit with your disability appeal letter.
Skilled legal counsel can make the difference in winning on appeal. To file a successful appeal, a disability attorney will help you prepare all necessary documentation, talk with your doctors, obtain statements from witnesses, consult with qualified vocational experts, and use the latest science and technology to investigate and build the details of your case.
A seasoned attorney will perform many tasks including:
- write the appeal letter to address every one of the insurance company’s allegations;
- contact medical and vocational experts to obtain assertive expert opinions;
- send you for a functional capacity exam or other appropriate medical exam;
- obtain updated medical records, and
- investigate the claims file to check for improper procedures or other discrepancies in the insurer’s handling of the claim.
A few of the legal strategies an attorney will use to put you in the best position to win your appeal are described below.
h3 id=”h-load-the-administrative-record”>Load the Administrative Record
Often the medical record alone is not sufficient to completely support an administrative appeal. How the medical evidence is introduced and demonstrated, or how an injury or illness has been described and portrayed is what really makes a difference.
During the administrative appeal process, medical records, medical literature and articles, doctor’s opinions, letters from friends or employers, photographs and all other types of evidence that document your impairments can be submitted and made part of the “record.”
In ERISA cases, once you have used up all appeals allowed under the policy, the “record” is closed. If a lawsuit against the insurer is necessary later on, no new evidence can be entered. The appeal is the only chance for you to submit key evidence of your disability into your case record.
That is why it is critical to fully load the record during the administrative appeal. A good lawyer will understand the importance and ensure that the record is loaded.
Note: Case law does show examples where additional evidence was added to the record after exhausting the administrative appeals and prior to filing suit against the insurer; however, this is not the norm.
h3 id=”h-validate-your-ltd-claim-with-vocational-expert-ve-opinions”>Validate Your LTD Claim with Vocational Expert (VE) Opinions
A vocational expert’s testimony and written evaluation can be a significant piece of evidence that can support your appeal and refute opposing statements from the insurance carrier.
Known as “jobs experts” or “VEs” for short, vocational experts generally have a master’s degree or a Ph.D. in the fields of Vocational Rehabilitation or Vocational Counseling.
The VE uses your Residual Functional Capacity (RFC), considers all restrictions and limitations caused by your impairments, as well as your age, education, background, work experience and skills, to form an expert opinion on what jobs you might be able to perform.
The VE could also come to the conclusion that there are no jobs available in the national or regional economy that you can do.
Some policies’ definition of “disabled” state that a claimant is disabled if he or she cannot find work that pays a certain percentage of their pre-disability income, usually around 60 to 80 percent. The vocational expert studies the local job market and wages and will conclude whether or not there are jobs that you can perform and still meet the salary percentage.
An example would be an orthopedic surgeon who performed skilled surgical procedures requiring fine dexterity and the ability to stand and bend over patients for hours, and now can only do sedentary work.
It is quite likely any sedentary job will not pay enough to reach the salary requirement. The disabled surgeon would meet the policy definition of disabled because the VE found that there are no jobs that the claimant could perform that pay 80 percent of his or her salary.
h3 id=”h-validate-your-ltd-claim-with-medical-expert-me-opinions”>Validate Your LTD Claim with Medical Expert (ME) Opinions
In the same way that the vocational expert reviews the record and forms an expert opinion, an independent medical expert can review all the medical records and form an opinion about your RFC.
A medical expert may also examine you and include those findings in the report. For instance, a medical expert opinion might be called for if there are not very many records or if the records do not accurately reflect your condition.
h3 id=”h-disprove-an-insurer-s-distortions-or-misuse-of-evidence”>Disprove an Insurer’s Distortions or Misuse of Evidence
When insurance claim examiners use only the evidence that supports a denial and ignores evidence that supports your disability, this is called “cherry-picking” the record.
For example, your doctor may write a letter stating that you are disabled due to back pain and can no longer work, but on a separate form may imply that you are able to sit for eight hours a day. The insurance company will disregard the “disabled” letter and state that your treating doctor has released you for work in a sedentary job because you can sit for eight hours.
A good lawyer knows this is going on and will ensure the proper evidence and expert testimony is in place if the insurance company cherry picks the facts in an attempt to block your claim.
h3 id=”h-refute-inaccurate-in-house-medical-reviews”>Refute Inaccurate In-House Medical Reviews
Insurers frequently employ in-house physicians or nurses who review a claimant’s medical records. A seasoned attorney will effectively argue against any misuse or misrepresentation of the evidence by the insurer during in-house medical reviews.
To recap, an experienced disability lawyer will be prepared for an insurance company’s denial tactics, and apply effective legal strategies to improve your chances of winning your claim:
- Load the Administrative Record
- Validate Your LTD Claim with Vocational Expert (VE) Opinions
- Validate Your LTD Claim with Medical Expert (ME) Opinions
- Disprove an Insurer’s Distortions or Misuse of Evidence
- Refute Inaccurate In-House Medical Reviews
Chapter 15: Insurer’s Tactics and Claim Denial
h3 id=”h-isolating-impairments-during-review”>Isolating Impairments during Review
Disability claimants frequently have more than one medical disorder. It may be a combination of impairments that causes a person to be disabled. However, during a file review, the insurance carrier’s hired doctors may focus on each disorder individually to find that the claimant is not disabled based on that one impairment.
It is common for the insurance company to send medical records to several doctors, each with a different “specialty.” When your medical disorders are separated out, the partial reviews do not reflect the complete picture of your disabling condition. Claimants end up with various expert medical opinions saying they are not disabled—but those experts have not even seen all of the conditions the person is actually dealing with.
h3 id=”h-use-of-video-surveillance”>Use of Video Surveillance
Insurance companies often hire private investigators to covertly film disabled claimants as they go about their day.
Some insurance companies videotape claimants after they have received benefits for a year or two. The insurance company will allege there are signs revealing that a claimant may be working or be capable of working, so an investigation is in order.
Often, the only type of activity that is filmed is a claimant going to a doctor’s appointment, going to the pharmacy or passing through a drive-through window. Yet, the surveillance is used to imply that you are able to perform more activity than originally reported, and therefore able to return to work.
This form of “evidence” has been used to terminate benefits even when a claimant’s record as a whole supports a finding of disabled.
h3 id=”h-hired-investigators-watch-you”>Hired Investigators Watch You
To create a reason to deny your claim or end benefits payments, many insurance carriers hire private investigators to follow and observe claimants. The aim is to catch them in an activity that they should not be able to do based on their disability claim.
The insurers state this is a way to reduce insurance fraud; however, it also results in deceptive practices on the insurer’s part in which it appears that a claimant is committing fraud when the truth is something completely different.
h3 id=”h-when-surveillance-leads-to-denial-of-benefits”>When Surveillance Leads to Denial of Benefits
Understanding how to handle video surveillance can be very important to your case, so you need to know what you are dealing with. The strategy behind using surveillance in a disability claim is this:
The insurance company sends the investigator’s reports and videos to the independent medical examiner (hired by the insurer) who will review your case. The goal is for the doctor to ultimately form medical opinions that oppose a decision that you are disabled. In effect, surveillance is a strategy to manufacture and manipulate evidence.
Whether taking a few photos or capturing your activities through sophisticated video observation, surveillance is not against the law – generally speaking as long as it is done in a public setting (i.e., not in your home or your business office), and when it does not violate a person’s reasonable expectation of privacy.
The question is, how does one deal with surveillance?
Watch the video. Request to view the footage so you know exactly how you are being characterized. You can then refute any footage that looks like it will hurt your claim with a clear explanation. Actions are often taken out of context, and the investigator might even edit the footage to make you look as though you are not disabled.
Read the reports. Are the investigators reporting the facts? Or, does their account of your actions contain editorialized descriptions intended to turn the reviewing doctor against you. It is not uncommon for an investigator’s report to hardly resemble the actual video footage.
What information did the claims examiner actually review? It often happens that the claims analyst does not take the time to watch the video recording. Instead, the examiner will read through the investigators’ reports. If the reports are infused with interpretations and opinions, the examiner who decides whether you are disabled is not getting a clear picture.
This is a situation in which an experienced disability lawyer can effectively argue that the insurance company failed to consider all the evidence when denying your claim.
Unless disability laws are revised to completely prevent surveillance, these steps become the only recourse a disabled claimant really has.
h3 id=”h-functional-capacity-exam-fce”>Functional Capacity Exam (FCE)
The Functional Capacity Exam is a set of physical tests that determine your Residual Functional Capacity (RFC)—your physical capabilities with regards to being able to work.
These standardized tests are administered by a physical therapist. The tests are done over a 3-4 hour period in a gym-like setting. You will be asked to walk on a treadmill, lift and carry cardboard boxes and submit to a series of different postures, including squatting and crawling.
The physical therapist observes and analyzes your physical abilities to sit, stand, walk, lift and carry.
These tests are designed to surmise the claimant’s maximum RFC in the work environment. However, 3–4 hours of activity cannot truly reflect how well a disabled doctor, chiropractor, carpenter or clerk would do eight hours a day, day after day, week after week.
Functional Capacity Exams can both help you or hurt you. When used properly, the FCE can provide excellent evidence of disability. Functional Capacity Exams can also be an upsetting and painful process for the claimant. When handled improperly, the FCE can produce unsound data that can actually be used against you to dispute the statements of the treating physician. Insurance policies are often written to require a claimant to endure an FCE.
h3 id=”h-malingering”>Malingering
If the insurer denies your claim because of “malingering,” this means the insurer believes you are faking or deliberately pretending to be disabled in order to avoid working and to gain financial benefits. Another term used by insurance companies for this sort of fraudulent action is “symptom exaggeration.”
An insurance company might claim malingering by saying that your symptoms do not equate with the objective evidence –therefore you must be overstating the pain or embellishing other symptoms.
h3 id=”h-grip-strength-and-malingering”>Grip Strength and Malingering
There are various procedures in use that unfairly identify disabled claimants who are not performing at maximum as “malingerers.”
An example is the grip strength test. During the FCE, you are asked to squeeze a handle rapidly, alternating hands. For a person with a normal or weak grip, the test results produce a bell shaped curve. The theory behind the grip test is that it is difficult for a person to consciously control how hard he or she grips the handle in a rapidly alternating exchange.
If the results are not bell-shaped, you will be charged with faking your hand strength. Worse still, the insurance company may claim you were malingering on all the tests. Despite the fact the FCE shows your RFC is very low, the insurer will claim that all FCE test results are invalid.
h3 id=”h-non-compliance”>Non-Compliance
If you refuse medical treatment or do not take medication as directed by your physician, that behavior is generally construed as being “non-compliant.”
Your insurance company may try to use your refusal as a means to deny a valid claim. This is an instance where an experienced attorney can apply the law to protect you and help you prove your decision or action was legitimate and based on justifiable grounds. There is a difference between choosing to not risk a surgery because of possible adverse outcomes or not being able to pay for medication, and non-compliance.
h3 id=”h-ignoring-the-treating-physician-s-opinion-relying-only-on-in-house-medical-reviews”>Ignoring the Treating Physician’s Opinion (Relying Only on In-House Medical Reviews)
An award of LTD benefits relies heavily on the evaluation of your medical condition. The extent to which an impairment prevents you from performing the material duties of your own occupation is paramount. Your treating physician’s medical opinion is an essential part of confirming the extent of your disability.
Insurance carriers may attempt to disregard or override the opinion of your doctor(s), and instead provide conflicting medical opinions using their own in-house physicians. Even though your treating doctor advised you to file for disability, has provided medical evidence that you are disabled and has continued providing your care and treatment – many insurers discount all of it and rely solely on their in-house doctor’s medical review.
If Your Administrative Appeal Is Denied:
Chapter 16: File an ERISA Lawsuit
h3 id=”h-who-can-file-a-lawsuit”>Who Can File a Lawsuit?
Any disability plan beneficiary or participant may file a lawsuit to enforce their rights under the plan or policy. This generally means the disabled individual but in some cases it could be a spouse, an estate or an heir.
h3 id=”h-who-is-the-lawsuit-against”>Who Is the Lawsuit Against?
A disability insurance lawsuit is usually brought against the “Plan” or the “Plan Fiduciaries,” often called the “Plan Administrator.”
It often happens that the plan administrator is the underwriting insurance company. For this reason, our disability guide often refers to the insurance company when talking about the Plan. More uncommonly, the proper defendant is the claimant’s employer.
The standard is: Who had the authority under the plan to grant or deny the disability claim?
h3 id=”h-where-do-you-file-your-erisa-lawsuit”>Where Do You File Your ERISA Lawsuit?
An ERISA lawsuit is filed in one of four locations:
- Where the Plan is administered;
- Where the breach occurred;
- Where the defendant resides; or
- Where a defendant may be found.
If you are the person bringing the lawsuit, you are the plaintiff. If the insurance company is being sued, it is the defendant.
As plaintiff, your choice of venue is given great deference by the courts. In cases concerning denied benefits, the courts typically decide that the breach of contract occurs where the benefits are to be received. Basically this means you may file your lawsuit where you live or expect your benefit checks to be delivered.
An ERISA case may be filed in either state or federal court, but the defendant will almost always transfer the case to federal court based on federal issue jurisdiction.
h3 id=”h-what-remedies-can-you-sue-for-under-erisa”>What Remedies Can You Sue For under ERISA?
ERISA law allows you to sue to
- “recover benefits due under the terms of the plan,
- to enforce rights under the terms of the plan, or
- to clarify rights to future benefits under the terms of the plan.”
The only possible remedy is for the Plan to be ordered to pay what it was obligated to pay you at the outset of your claim, along with an award for retroactive benefits.
No additional contractual compensatory damages or punitive damages are permitted in ERISA claims. You may also seek a declaration of a right to future benefits or an injunction preventing a future denial of benefits.
h3 id=”h-how-much-time-do-you-have-to-file-an-erisa-lawsuit”>How Much Time Do You Have to File An ERISA Lawsuit?
A deadline known as the “Statute of Limitations” will dictate by when your lawsuit must be filed. If you do not file suit before the statute of limitations expires, your claim is lost forever. This is unconditional. One day late and your claim is gone.
NOTE: ERISA maintains no statute of limitations directly, so instead you must look to each individual state for the appropriate deadline. Most courts apply a breach of contract statute of limitations to a benefit denial claim under ERISA. For example, in Texas the deadline would be four years from the date of breach or denial. Deadlines vary from state to state.
Also be aware that your insurance plan or policy may shorten the deadline as stated in the terms of the plan. It is essential that you review all of your plan documents for forthcoming or imminent deadlines. Plans often shorten the deadline to three years from the date by which proof of disability must be provided. Other plans implement even shorter deadlines.
h3 id=”h-before-you-can-file-a-lawsuit-you-must-exhaust-your-administrative-appeals”>Before You Can File a Lawsuit: You Must Exhaust Your Administrative Appeals
Under ERISA law, all Employee Benefit Plans are required to have in place an internal administrative appeal procedure. Before you have a right to file a lawsuit, you must first appeal the denial by exhausting the disability plan’s administrative remedies.
You must not skip this step! If you do you will lose your right to file your lawsuit.
Typically the final paragraph or two of the insurer’s denial letter explains the deadline for filing the administrative appeal. The deadline is generally 180 days from the date of the denial letter.
Once the insurer makes the final denial of an administrative appeal, no further evidence may be submitted to your claim. In the lawsuit, the court will basically be reviewing the stacks of medical records, vocational records, job history and other records that you developed and submitted in the administrative appeal.
If you did not do a first rate job developing your evidence at this point, you will likely not have a good chance in Court.
h3 id=”h-in-an-erisa-lawsuit-what-must-you-prove”>In an ERISA Lawsuit, What Must You Prove?
Winning your ERISA lawsuit calls for far more than just proving you are disabled. You now must show that the insurance company “abused their discretion” in denying your claim based on the evidence available to them at the time they made their final decision of denial. That is why it is essential to completely develop your case during the administrative appeal.
Proving both a structural conflict of interest and an individual conflict of interest with the insurance company and its decision makers is a critical part of the litigation. The odd procedure set up under ERISA allows the insurance company to decide if they have to pay the claim, assuming that their financial self-interest won’t outweigh their fiduciary duty to do the right thing.
In previously litigated cases, it has also been discovered that insurance carriers sometimes create financial incentives for their own doctors, vocational experts and decision makers to keep claim cost down. These inherent conflicts of interest must be demonstrated to the court when litigating these cases. Doing so can cause the court to use a more favorable “sliding scale” when deciding these cases.
Some states are beginning to attempt to remove or void language in insurance contracts that give the insurance carrier complete “discretion” in deciding claims. If this trend continues and is upheld by the federal courts, it would ease the claimant’s burden of proof before the federal court. This will vary from state to state and is another reason to consult an experienced ERISA attorney early in the process.
h3 id=”h-the-possible-outcomes-in-an-erisa-lawsuit”>The Possible Outcomes in an ERISA Lawsuit?
Depending on the strength of your case, the most likely outcomes in an ERISA lawsuit are:
- Settlement
- Motion for Summary Judgment
- Bench Trial
- Remand for Another Administrative Appeal
Settlement: It may be possible to negotiate a “buy out” with the insurance carrier to settle the claim and surrender the policy;
Motion for Summary Judgment: The case could be decided for or against you based on a Motion for Summary Judgment filed either by yourself (through your attorney) or by the insurance carrier. A motion for summary judgment is filed by either party when they believe the case could be decided by the judge “as a matter of law” without the need for a trial. Remember, there is no opportunity to submit new evidence to the court, therefore the only thing the judge needs to consider to decide the motion for summary judgment is the evidence already submitted (referred to as the administrative record).
Bench Trial: The judge could decide to have a bench trial. Since there is no right to a jury trial, the case would be tried to the judge at the “bench.” The judge would indicate what issues were not decided on the motions for summary judgment and that would dictate what live testimony may be needed for the judge to decide the remaining issues.
Remand for Another Administrative Appeal: The judge could order the case remanded back for another administrative appeal to develop the case further.
One thing to remember is that if a judge rules in your favor, he or she only has the power to order the insurance company to pay you the back benefits you are owed and to start your monthly benefits from this point forward. The insurance company has the right to require you to continue to demonstrate that you are disabled per the policy definition and could conceivably cut you off again in the future. The judge may award you some attorney fees as well.
Chapter 17: File a Lawsuit on an Individual (Non-ERISA) Disability Insurance Claim
If you purchased a disability policy privately and you believe your carrier has wrongly denied your claim, you have far more legal recourse than claims subject to ERISA law.
Each insurance litigation case is unique. Some insurance cases can be settled without going to court; others may require a trial to resolve the dispute.
A lawsuit against an insurer for privately purchased LTD insurance is governed by state laws. You are entitled to all procedural rights and remedies available to you in your state—just like you would under your privately purchased homeowner’s or life insurance policies. You will retain the right to a jury trial and the right to present evidence and cross-examine any witnesses testifying for the insurance company.
In cases where an insurance carrier has denied a claim, most states have multiple remedies available if litigation is necessary. What applies to all state law claims is that you should endeavor to give your insurance company every opportunity to do the right thing and put it in writing.
Many states require that you put your grievances in writing and establish a certain amount of time that must be given for the insurance company to comply. If the insurance company fails to comply with your requests by the statutory deadlines, you probably have many extra contractual remedies available to you that would not be available if your case was ERISA preempted.
h3 id=”h-contractual-remedies-that-may-be-available”>Contractual Remedies that May Be Available
These contractual remedies include causes of action for
- Breach of contract
- Bad faith
- Punitive damages
- Mental anguish or consequential damages
- Loss of credit
- Deceptive Trade Practice Act damages
- Insurance Code Violations
- Attorney fees
In a lawsuit seeking private LTD benefits, you also have rights that are not available under ERISA law:
- You are allowed a trial by jury,
- You may engage in discovery of relevant evidence from the insurance carrier,
- You may cross-examine any witnesses the insurance company puts on the stand to testify against you.
h3 id=”h-breach-of-contract-of-a-private-disability-insurance-claim”>Breach of Contract of a Private Disability Insurance Claim
Under a breach of contract claim, your attorney must prove that the insurance company essentially disobeyed the insurance policy by failing to concede that you are disabled as per the terms of the policy.
Breach of contract lawsuits often center on the policy’s wording and terms to demonstrate what obligations each party had, and whether the parties met those obligations. Your lawyer will work to have the insurer pay compensatory damages (the value of actual denied benefits and any incidental damages.)
h3 id=”h-bad-faith-in-private-disability-insurance-claims”>Bad Faith in Private Disability Insurance Claims
Did the insurance company breach the covenant of good faith and fair dealing by denying your claim?
Did the insurance company intentionally act to cause harm, or deliberately ignore the risk of causing harm?
If there was no reasonable basis for the denial under the policy, the insurance company breached the insurance contract in an act of “bad faith.”
Typical signs of bad faith actions are when the insurance carrier
- misrepresents the provision and coverage in the policy
- does not acknowledge your claim or reply to you promptly upon notification of a claim
- does not investigate your claim promptly and thoroughly
- tries to make you settle your claim for much less than it is worth
- alters any part of the policy without your knowledge
- denies your claim without explanation
- delays or denies payment without a reasonable basis
- applies unreasonable misinterpretations of policy language
Verdicts of bad faith insurance may result in the award of monthly disability benefits, plus punitive damages, together with litigation costs and attorneys’ fees. The jury will consider the amount of harm caused, motive, and other factors of the case.
Meticulous preparation and understanding the methods used by powerful insurance firms is the key to success. If you have such a claim, bringing in an experienced attorney early will help you “set up” your case for a good result down the road.
Chapter 18: Legal Representation during Your Lawsuit
Disability insurance is big business. While selling the plans and receiving premiums is profitable, paying on claims is not.
Many companies use strategies and tactics that enable them to deny or stop payments on valid claims. Their hope is that eventually you give up and abandon the claim, or otherwise fail in your efforts to appeal the claim.
An experienced attorney is well aware of all the tactics an insurance company uses during the administrative appeal process to turn down a claim. Many of these tactics have been litigated in prior lawsuits.
An attorney researches case law in a claimant’s jurisdiction and uses that law to support legal argument to persuade the judge that the insurance company made the wrong decision in finding the claimant not disabled.
Remember, in long term disability lawsuits under ERISA, there is no jury trial, only a trial before a judge, called a bench trial. The judge reviews written legal argument, called a Motion for Summary Judgment, to make a decision. It is important to have an attorney knowledgeable in the appropriate case law during the lawsuit.
An attorney understands the strengths and weaknesses of a case and may be able to negotiate a cash settlement on behalf of the claimant before it is necessary to present argument to a judge.
Chapter 19: How Does an Attorney Get Paid?
There are a number of ways to hire an attorney. They range from a traditional hourly basis, to a pure contingency fee arrangement where the attorney is compensated from the proceeds of the case and the disabled claimant does not owe attorney fees unless the claim is successfully resolved, or some combination of both.
The difference generally boils down to who is taking the risk of whether a recovery is made: the client or their attorney. If you hire an attorney on an hourly basis, you are taking all the risk of an unfavorable outcome. In other words the claimant has to pay attorney fees whether they win or not.
Under a contingency fee arrangement, the risk of not getting paid shifts to your attorney. In other words, the attorney will not get paid if the claim is not successful.
Most claimants hire their lawyer on a contingent fee basis. Generally speaking, an attorney expects to get compensated more for doing contingency fee work because the attorney is assuming a risk that they will not get paid at all.
h3 id=”h-can-you-recover-attorney-fees”>Can You Recover Attorney Fees?
In the case of ERISA lawsuits, the answer is “Maybe, but it is difficult.” Generally speaking, attorney fees are not recoverable in most causes of action without an explicit statute authorizing it.
ERISA does allow for recovery of attorney fees, but only at the “discretion” of the judge. In other words, it is not mandatory that the judge award attorney fees and the judge also has the discretion to award what he thinks is reasonable, not necessarily what you have to pay.
This is especially evident given that most claimants hire their attorney on a contingent fee basis, but the judge can only award fees based on a reasonable hourly rate.
Also, the judge will not award attorney fees based on work done during the administrative appeal even though the claimant still has to pay them. In short, ERISA strikes again.
Conversely, a lawsuit against an insurer for privately purchased LTD insurance is governed by state laws. In these cases, the prevailing disabled claimant is generally entitled to recover attorney fees from the insurance company.
h3 id=”h-how-fee-awards-are-calculated-under-erisa”>How Fee Awards Are Calculated Under ERISA
It is very difficult to get the opposing side to pay the attorney fees in an ERISA lawsuit. However, some judges are fairly responsive to this practice and even adhere to the rule posed in other types of cases (but missing in ERISA) that the winning party deserves to have the losing side pay.
With this in mind, it is helpful to understand the basics of how the actual amount of your monetary award is calculated.
h3 id=”h-computing-lawyer-fees-using-the-lodestar-method”>Computing Lawyer Fees Using the Lodestar Method
Lawyers’ fees are primarily calculated by what is known as the Lodestar method. The court determines the fees by multiplying an equitable hourly rate by an equitable number of expended hours.
To get the lodestar figure, the district court has to look at 12 lodestar factors.
- How much time and labor was involved.
- How unique and/or difficult the questions raised in the case were.
- How skilled the attorneys needed to be to handle the case.
- How much work the attorneys gave up by taking this case.
- The amount of the attorneys’ typical fee.
- Whether the fee is contingent or fixed.
- Time limitations present – imposed either by circumstances or the client.
- The overall amount involved and what was obtained.
- The attorneys’ ability, reputation, and experience.
- The case’s “undesirability.”
- How long the attorneys have been working with the client.
- How much was awarded in similar cases.
By resolving all the above factors as required by the ERISA statute, the judge should arrive at a suitable award amount. Not all parties may agree with this determination, but it is how long term disability cases work.
By being aware of all twelve factors, you may have a better sense of what might happen in your case.
Chapter 20: Getting Legal Representation: What to Look For
Statistically, claimants stand to double their chances of winning their disability case if they retain an attorney qualified to help them file a claim or appeal a denied claim. When complex ERISA disability laws take over; choosing the right lawyer can make the difference in living in hardship or getting the benefits you deserve.
An attorney who will deal efficiently with medical and vocational experts, anticipate insurance company tactics, who is in his or her element arguing ERISA regulations and appearing before the federal judicial system is essential to developing a rock-solid appeal and capable of reversing a denial and winning benefits.
The following are things you should know about any attorney before you hire them:
h3 id=”h-know-the-attorney-s-competence”>Know the Attorney’s Competence
First you want to know if the lawyer is qualified, so ask:
Is he or she a licensed attorney? This may sound like an odd question, but you do not have to be a licensed attorney to handle administrative appeals under ERISA regulations – and there are in fact some people out there who will handle your administrative appeal for a fee. They can handle administrative reviews but cannot take your case to federal court if necessary.
How many years of experience does the attorney have handling ERISA based disability insurance claims? Again, this area of law is complex so you want someone with vast experience. You want to talk with an attorney who has prevailed against billion-dollar insurance companies in settlements and lawsuits. You also should dig a little deeper than just years of experience.
How many individually owned disability insurance cases has the attorney handled? Look for an attorney who has built his or her reputation on assisting medical professionals, CEOs, key executives and other high wage earning individuals with their private disability insurance claims. The legal counsel you hire should have authoritative knowledge and years of experience negotiating and litigating these claims.
A related question is whether or not disability law is the main focus of their practice. Many attorneys are general practitioners that handle many areas of law such as wills, probate, family law, criminal matters as well as some insurance claims work.
ERISA claims are complex and require an ERISA specialist. Bad faith insurance and breach of contract issues demand an insurance attorney’s expertise of the law and the insurance industry.
Another good question to ask is have they written on the subject and if so, will they share this material with you? Often experienced attorneys will have written papers, articles, editorials or books on their area of expertise. These can demonstrate an in depth knowledge about the subject. Many times good attorneys will put this material on their websites so you can check it out in advance. They may also post Videos, blogs or other materials that can be helpful.
h3 id=”h-investigate-the-attorney-s-reputation”>Investigate the Attorney’s Reputation
Once you have established that an attorney has the necessary experience, you want to explore their reputation. Go to the internet and see if they have any reviews on Google, Yahoo or Yelp. Do not be put off by an occasional negative review; not every claimant wins, and sometimes they take it out on their lawyer. But look for patterns or trends in the reviews.
Next, go to Martindale.com and check out their attorney ratings. Martindale.com is the gold standard for lawyer ratings as it has been around in one form or another for over 140 years. Martindale conducts peer review surveys, asking lawyers to rate other lawyers anonymously. The areas surveyed are a lawyer’s legal knowledge, analytical competence, judgment, communication ability and legal experience. Lawyers are then rated on a 5 point scale. Lawyers that rate 4.5 or above are designated with an AV Preeminent rating, which the best rating possible. Those from 3.0-4.4 are designated BV Distinguished and below that are designated as Peer Review Rated.
Another good source is to go to Avvo.com and check out their AVVO rating and reviews. AVVO does a great job of rating lawyers on a 10 point scale, weighing an attorney’s experience, industry recognition and professional conduct. Former clients and other lawyers can leave reviews at AVVO as well.
Super Lawyers is another ratings service of outstanding lawyers by practice area for those lawyers that have achieved a high degree of peer recognition and professional achievement. Go to Superlawyers.com to find out if a particular lawyer has been designated a “Super Lawyer.”
Finally, you might also inquire about their honors, recognitions and organizational memberships.
Top of LTD Guide
References
- ERISA § 502(a)(1)(B). (Pub.L. 93–406, 88 Stat. 829, enacted September 2, 1974, codified in part at 29 U.S.C. ch. 18)
- 29 U.S. Code Chapter 18 – EMPLOYEE RETIREMENT INCOME SECURITY PROGRAM; https://www.law.cornell.edu/uscode/text/29/chapter-18 , accessed July 18, 2016.
- Marc Whitehead, Disability Insurance Policies: How to Unravel the Mystery and Prove Your Claim. Accessed July 18, 2016. /disability-insurance-policies-ebook/
- Marc Whitehead & Associates, Attorneys at Law, LLP. A National Disability Claims Law Firm. Accessed July 18, 2016. /
Table of Contents: Social Security Disability
Guide to Social Security Disability Insurance (SSDI) / Supplemental Security Income (SSI)
Chapter 2: Available Social Security Programs: SSDI & SSI
Chapter 3: Can I Get Retroactive Payments (“Back Pay”) for SSDI & SSI?
Chapter 4: Is there a Waiting Period for SSDI & SSI?
Chapter 5: How to Apply for Social Security Disability Benefits
- How Long Does It Take to Get Social Security Disability Benefits?
- How Does Social Security Decide You are Eligible for Disability Benefits?
Chapter 6: The Social Security Appeals Process: What to do if a Claim is Denied
Chapter 7: The Administrative Law Judge (ALJ) Hearing
Chapter 8: Developing Your Social Security Disability Case
Chapter 9: The 5-Step Process for Proving You Are Disabled
Chapter 10: Step One – You Are Not Gainfully Employed
Chapter 11: Step Two – Proving You Have a Severe Impairment
Chapter 12: Step Three – Proving Your Impairment Meets or Equals a Medical Listing
Chapter 13: Residual Functional Capacity (RFC)
Chapter 14: Step Four – Proving You Can’t Do Your Past Relevant Work
Chapter 15: Step Five – Proving You Cannot Do Any “Other Work”
- It Is SSA’s Burden to Establish Your Ability to Perform Other Work
- Use of the Medical–Vocational Guidelines (Grid Rules) to Determine Disability
- Using the Grid Rules to Direct a Finding of “Disabled” or “Not Disabled”
- How Your Age Affects the Application of the Grids
- Education and Illiteracy in the Grids
- Job Skill Levels in the Grids
- Loss of Hands and Finger Use and Your Ability to Perform Unskilled, Sedentary Work
- Past Work Experience: Are Your Skills Transferable?
- Vocational Expert Testimony Is Used When Grids Are Not Applied
- Job Availability in the National Economy
- Structure of the Medical-Vocational Guidelines (Grids)
- The Grids: Maximum RFC Permitted for Disability Finding
- Grids as a Framework for Decision Making
- RFC for Less Than a Full Range of Sedentary Work
- Nonexertional Limitations
- Work Skills that can Transfer to Another Job
Chapter 16: Getting Help with Your SSDI Claim
- Attorney vs. Non-Attorney Representation
- What Will a Qualified SSDI Attorney Do For Me?
- What Will an SSD Advocate (Non-attorney) Do For Me?
- Expenses Are the Same for Attorney and Non-Attorney Representatives
- Where to Find an SSD Attorney or Non-Attorney Advocate
Chapter 17: Winning Social Security Disability: What Happens Next?
- Do I have to do anything in order to receive my payments?
- When will SSA start paying me?
- How far back will SSA pay me benefits?
- What will the amount of my monthly check be?
- Will I receive a notice from SSA explaining my benefits?
- When will the Notice of Award come in the mail?
- Should I wait until I receive the Notice of Award before I cash my check for past due benefits?
- Why would there be a problem if I was overpaid?
- When will my regular monthly benefits begin?
- Will I be eligible for Medicare?
- The decision cover sheet says that the appeals council may review the decision “On Its Own Motion.” What does this mean?
- Will I have to pay taxes on the Social Security disability benefits I receive?
- What is a “Continuing Disability Review (CDR)?”
- What will I have to do for a Continuing Disability Review?
- What if the SSA finds that my disability has ceased, but I’m still not able to work?
- What can I do to make sure my disability benefits will continue?
- Is it as hard to keep my benefits as it was to get them in the first place?
- What can I do to make working with SSA easier?
Guide to Social Security Disability Benefits
Chapter 1: Introduction
Each year, disabling medical conditions prevent countless U.S. taxpayers from working and earning a living. As a result, Federal assistance programs exist to help the disabled during difficult financial times.
These disability programs are administered within the federal Social Security Administration (SSA). The largest disability income programs include
- Social Security Disability Insurance (SSDI or SSD)
- Supplemental Security Income (SSI)
Social Security benefits are not awarded automatically. You must apply to get them. Whether you are eligible for benefits relies heavily on the medical evidence of your impairment and your vocational ability.
h3 id=”h-ssa-definition-of-disabled”>SSA Definition of Disabled
The Social Security Act defines a disability as:
- the inability to engage in any substantial gainful activity (SGA) by reason of any medically determinable physical or mental impairment that can be expected to result in death, or which has lasted or can be expected to last for a continuous period of not less than 12 months.*
The Act states that you (as a claimant) will be found disabled only if
- your impairment(s) is of such severity that you are not only unable to do your previous work but cannot – considering age, education and work experience – engage in any other kind of substantial gainful work that readily exists in the national economy.*
*Source: SSA Website, Disability Evaluation under Social Security
h3 id=”h-a-better-chance-of-winning-social-security-disability-benefits”>A Better Chance of Winning Social Security Disability Benefits
Like other government programs, the SSA has standards that regulate who might qualify for benefits.
Qualifying for Social Security Disability (SSD) is not easy, and many claims are denied. This is because the Social Security regulations are quire complex. Most people don’t fully understand the extent of proof required by the SSDI and SSI programs. If a case is poorly developed, the SSA is not able to award benefits.
This results in worthy applicants being denied benefits >> appealing >> being denied again >> appealing again.
Statistics show extremely low approval rates for Social Security Disability applicants, averaging 38 percent for initial claims filed from 2003 to 2012.
Plus, after receiving a denial, the number of claimants dwindles. Most applicants either give up out of frustration, or they do not receive qualified help, or they are simply too disabled to bear the burden of pressing their claim on appeal.
For every 1000 claimants filing an initial application, once denied, only*
- 312 applicants move on to appeal for Reconsideration
- 185 applicants continue further to appeal to the ALJ Hearing Level
- 37 applicants continue further to appeal to the Appeals Council
Yet while the numbers sound dismal, the percentage of awards increase to 55% at the ALJ Hearing level of appeal.
*The Social Security Disability Appeals Process
h3 id=”h-your-right-to-representation”>Your Right to Representation
Every person has the right to be represented by an attorney or other qualified representative while pursuing a claim under the Social Security Act.
You may appoint a representative to assist you in all aspects of your claim. This can be critical to developing a case that will stand up to the rigors of SSA evaluation, rules and deadlines.
An SSA representative, whether attorney or non-attorney, is required to charge for their services only if your claim is approved. Fees are regulated by law.
Learn more about getting qualified help with your disability claim.
h3 id=”h-do-not-give-up”>Do Not Give Up!
The purpose of this guide is to help you overcome the tough challenges that lie ahead when applying for Social Security disability benefits. Our information will help you understand the complex rules and procedures, so you can make informed decisions and move forward with a well-prepared claim.
Chapter 2: Available Social Security Programs: SSDI & SSI
This guide addresses:
- Social Security Disability Insurance program (referred to as SSDI or SSD), under Title II of the Social Security Act
- Supplemental Security Income program (SSI), under Title XVI of the Social Security Act
h3 id=”h-social-security-disability-how-it-works”>Social Security Disability – How It Works
Social Security disability is designed to financially help qualified disabled individuals who need Social Security benefits earlier than they would typically be entitled to them.
The qualifying age in 2015 was generally age 66, with some exceptions based on the year you were born (you can visit the Social Security website for their chart on full retirement age).
SSD works similar to an insurance plan for workers. Much like when you pay premiums for a private insurance policy, you qualify for SSD only if you have worked and paid Social Security taxes into the program’s Trust Fund over a set amount of time.
You must also have contributed to the program recently enough to have disability “insured status.” This is one of the main reasons it is important to apply for benefits as soon as you are able to after an incapacitating disability.
h3 id=”h-your-contributions-to-social-security-quarters-of-coverage-qc”>Your Contributions to Social Security – Quarters of Coverage (QC)
Contributions are counted in quarters of coverage, or QC. One QC = 4 months, and you cannot earn more than 4 QCs per year. QCs are sometimes referred to as Social Security “credits.”
The minimum earning requirements have gone up every year since 1978.
To qualify for SSDI: As a rule, you must have one quarter of coverage for every calendar year after the year in which you turned 21, up to the calendar year before becoming disabled.
The rule for disability insured status for those over age 31 is that you must have 20 QCs out of the 40 calendar quarters before becoming disabled. This is often called the 20/40 rule. It is usually satisfied by evidence of significant work in five out of the last 10 years.
For someone who has a steady work record, insured status will lapse about five years after stopping work. If this is the case, you will have to prove that you were disabled before the date you were last insured.
There is a reduced quarter of coverage requirement for those who become disabled before age 31.
h3 id=”h-what-if-ssa-says-you-have-not-earned-enough-qcs”>What if SSA Says You Have Not Earned Enough QCs?
What you can do:
- Apply for SSD or SSI even though Social Security says you are not eligible based on not having enough quarters of earned credit. It may be possible for you to amend up to three years of tax returns in order to gain quarters of credit. This also applies to claimants who are self-employed. A tax professional or other qualified individual should be able to assist.
- Also, as with a private insurance policy, there will be a lapse in insurance status with SSD after a person either stops working or stops paying Social Security taxes.
h3 id=”h-are-you-eligible-for-ssd”>Are You Eligible for SSD?
You qualify for Social Security disability through
- Insured Status: As explained above, you have worked and paid Social Security taxes over a set amount of time.
- Current Income: At the time you apply for SSD, you must either have stopped working completely or have only a minimum amount of income. The income amount tends to vary each year.
- Medical Condition: The final qualifying component is your disabling medical condition. Your illness or injury must be severe enough to limit basic abilities, such as lifting, standing, walking, or remembering.
You are also considered eligible for SSD if you are disabled to the point that you absolutely cannot perform a current job or train for another type of work. There are further considerations involved in determining whether a blind claimant is eligible for disability benefits.
If you win a disability claim under the SSD program, you are entitled to benefits that accrue five months after the onset of your disability, in addition to monthly disability payments in the future.
h3 id=”h-supplemental-security-income-ssi”>Supplemental Security Income (SSI)
Supplemental Security Income (SSI) helps those who have limited assets with which to support themselves.
SSI is a federal welfare program that is paid out of general revenues. This is different from the SSDI benefits that are paid out of the Social Security trust fund.
A person who is disabled, blind or over the age of 65 may qualify for SSI benefits.
Your State May Supplement SSI: The SSI benefit amount awarded per month varies from state to state because some states supplement the federal SSI benefit.
h3 id=”h-who-is-eligible-for-ssi”>Who Is Eligible for SSI?
In order to be eligible for SSI,
- You must be a U.S. citizen or fall into a group of limited exceptions to the citizenship rule;
- You must be disabled based on the same criteria and definition of disability as used for SSDI;
- SSI program has specific income and asset requirements that must be met;
- You must file an application to be considered.
h3 id=”h-what-are-ssi-income-and-asset-limits”>What Are SSI Income and Asset Limits?
Because SSI pays benefits based on financial need, there are limits placed on your income and assets.
Income refers to money you get from wages, Social Security benefits and pensions, as well as food and shelter. Income limits also vary by state, so the monthly income you are allowed to receive and still qualify for SSI depends to this extent on where you live.
Assets are the things you own such as stocks and bonds, bank accounts, real estate, or cash. In order to qualify and continue to be eligible for SSI, an individual can have no more than $2,000 in assets and a couple can have no more than $3,000 in assets.
Certain assets, such as your home, or one car if it is used for work or transport for medical care, are excluded.
Knowing which assets might not count in your circumstances is important, so it is a good idea to discuss this with a qualified representative who knows yours specific situation.
h3 id=”h-common-law-marriage-can-affect-ssi-eligibility”>Common Law Marriage Can Affect SSI Eligibility
Your SSI benefit amount is based on many factors, including marital status.
Before you mistakenly declare to SSA that you are “common-law married,” make sure this is the case under your state’s marriage laws. SSA follows state laws in these cases.
This is important because the income of a valid legal spouse may prevent a claimant from qualifying for SSI. Not all states address the legality of common law marriage, and one state’s statutes will be different from another.
Chapter 3: Can I Get Retroactive Payments (“Back Pay”) for SSDI & SSI?
SSDI:
Social Security disability might be paid retroactively for up to 12 months before the date you actually applied, if all requirements are met. This retroactive pay is only considered when a first-time claimant is entitled to at least one month of benefits during the 12-month period, which establishes a period of disability.
The period of disability is yet another reason it is essential to apply for Social Security disability benefits as soon as possible.
SSI:
SSI benefits cannot be retroactive.
Chapter 4: Is there a Waiting Period for SSDI & SSI?
SSDI:
Social Security disability has a five-month waiting period after the onset of the disability, in order for Social Security disability benefits are payable. No Social Security disability benefits to be payable in that time period.
It is important to note that SSA only considers full months. This means that the actual waiting period might be longer than five months unless you become disabled the first day of the month of a waiting period.
SSI:
The effective waiting period for SSI is the first of the next month after all requirements are met, (versus the minimum five months required for SSD). It is therefore possible to first receive SSI benefitsquicker than SSD payments.
Chapter 5: How to Apply for Social Security Disability Benefits
SSD and SSI benefits should be applied for immediately to prevent the possibility of losing any benefits to which you are entitled.
There are several ways you can apply for Social Security benefits.
- Apply Online: You can apply for both SSD and SSI online at www.SSA.gov.
- In-Person: You can file a claim in person at the local district and branch Social Security office in your area.
- Phone: To apply by telephone, call the Social Security office at (800) 772-1213.
- For SSI applications, a human resources official at the local hospital or clinic in which you were diagnosed may be able to assist with the initial application process.
When applying, a key to making your case for disability as strong as possible is to emphasize how difficult it was for you to physically or mentally perform your job. Social Security’s main concern is whether you are able to work in a full time capacity in any kind of employment.
Be prepared to provide detailed answers to questions regarding your
- Past work – how you describe your previous work experience can affect the outcome of your claim*
- Medical conditions
- Education
- List of your doctors and current contact information
- List of prescriptions
*Do not underestimate how much time you spent walking, standing, or lifting impacted your health. Be specific and detailed on your job duties.
h3 id=”h-how-long-does-it-take-to-get-social-security-disability-benefits”>How Long Does It Take to Get Social Security Disability Benefits?
The initial determination process usually takes from 90 to 180 days, so assume an average of 120 days for SSA to reach an initial decision. Unfortunately, the majority of cases are denied at this step.
The initial application starts at your local SSA office. The application is processed through the SSA Field Offices, and also by Disability Determination Services (DDS) which are typically located in your state.
At this point, trained SSA examiners are responsible for compiling all medical, non-medical and vocational evidence, reviewing your case, and making the initial determination on whether you meet SSA’s definition of disability.
h3 id=”h-how-does-social-security-decide-you-are-eligible-for-disability-benefits”>How Does Social Security Decide You are Eligible for Disability Benefits?
Social Security determines disability using a Five Step Evaluation Process. Each step is a question that tries to determine the significance and measure of your impairment, and how it affects your ability to work full time.
The Five Step Evaluation Process is a sequential process. This means that if at any step you are determined either disabled or not disabled, the process stops and disability is either awarded or denied.
The five steps are:
- Are Your Gainfully Employed?
- Do You Have a Severe Impairment that Will Last 12 Months or Result in Death?
- Does the Impairment Meet or Equal the Severity of a Defined Medical Listing?
- Are You Able to Perform Your Previous Type of Work?
- Are You Able to Perform Other Generally Available Work?
Learn more about the Five Step Evaluation process here.
As an applicant, you can be found disabled if you
- have a listed impairment (SSA uses a specific Listing of Impairments that are considered disabling),
- have a severe impairment that is equal to a listed impairment,
- have a severe impairment when medical and vocational factors are considered, or
- had a previously established entitlement to a disability benefit.
You can be denied benefits if you
- have an impairment that is not expected to last 12 months,
- have an impairment that is not considered severe,
- are able to perform your usual type of work, or
- are able to perform another type of work.
SSA may also deny benefits if you:
- have an impairment resulting from drug addiction or alcoholism
- provide insufficient medical evidence,
- fail to cooperate,
- fail to follow prescribed treatment,
- do not want to continue development of your claim, or
- return to substantial work before disability can be established.
Source: SSA.gov: Outcomes of Applications for Disability Benefits
Chapter 6: The Social Security Appeals Process: What to do if a Claim is Denied
If SSA denies your disability claim, you have the right to appeal the decision. You have 60 days to appeal for the first level of appeal.
Your notice from SSA will provide instructions about how to appeal the decision. Appeal means you send the unfavorable decision back to SSA for official reconsideration.
Begin by calling your local SSA office to inform them you need to appeal the SSA’s decision for benefits. SSA will send the appropriate forms that must be completed and instructions of what SSA needs.
You may also appeal a decision online through SSA’s website.
h3 id=”h-four-steps-in-the-appeals-process”>Four Steps in the Appeals Process
The appeals process has four levels. Any time your claim is denied on any of the four levels, you must appeal to the next level in a specified time limit. Otherwise your claim is dismissed and you will have to start all over.
Even when all administrative appeals are exhausted, it is still possible for you to pursue benefits by filing a lawsuit in a local federal court requesting the court review the matter to determine if you have received a fair hearing.
There are four steps to the appeals process. What happens at each step, and the approximate time each step lasts, are as follows:
Step One: Reconsideration—about 90 days
If your initial application is denied, you have 60 days to appeal for a Request for Reconsideration.
The Reconsideration stage becomes the first level of appeal. In this step you are basically asking SSA for a 2nd opinion.
A new SSA examiner is assigned to your case, and you are able to submit any new medical and vocational evidence to support your claim.
Unfortunately, most appeals at the reconsideration stage are denied.
If denied, you have 60 days to appeal for a request for an ALJ Hearing.
Step Two: Hearing before an administrative law judge (ALJ)—about 530 days
The ALJ hearing is probably the most important level of the appeals process and gives you the best odds of winning.
Like a scaled-down trial, you have the opportunity to present your case to an actual judge who will decide whether you are disabled. You can present new evidence, including witness testimony.
The biggest mistake SSDI claimants make is not appealing to this third level of appeal.
If denied, you have 60 days to appeal to the Social Security Appeals Council.
Step Three: Review by the Appeals Council—about 270 days
New evidence may be introduced at this stage. If you have no new evidence, the Appeals Council (AC) will review the ALJ’s decision for procedural error. The Appeals Council is located in Falls Church, VA.
The Appeals Council may:
- Award benefits (overturning the denial decision);
- Send your claim back to the ALJ for a new decision;
- Deny the request for review, or refuse benefits.
This is the final level of Administrative Review for the SSA. If your claim is denied at this step, you must file an appeal in federal district court within 60 days.
Step Four: File a Federal Lawsuit—about 540 days
You may file a lawsuit in a federal court district if you do not agree with the decision from the Appeals Council. This can take up to two years in addition to the time taken in steps one through three, plus the 120 days of initial determination.
h3 id=”h-you-have-limited-time-to-file-an-appeal”>You Have Limited Time to File an Appeal
Once the SSA denies your application for benefits, the clock is ticking.
With one exception, the allotted time for all Social Security appeals is 60 days from the date of receipt of the decision of denial. SSA presumes you receive notice of their decision in the mail 5 days after the date on the notice.
The one exception to this 60-day rule is: You have only 30 days to file exceptions with the Appeals Council in a case remanded by a Federal court.
What is a federal court remand? If you appeal an unfavorable decision to federal court, and federal court agrees you did not get a complete and fair hearing—federal court will send the case back (remand the case) to the ALJ for a new hearing. The time limit for this process is 30 days.
h3 id=”h-what-if-you-missed-your-60-day-deadline”>What if You Missed Your 60-Day Deadline?
If you miss the 60-day window to appeal, you must go back to the beginning and file a new application.
h3 id=”h-reopening-time-limits-based-on-good-cause”>Reopening Time Limits Based on “Good Cause”
If you have a valid reason for being late in filing your appeal, you may still be allowed to file if you can show “good cause.” SSA may permit a detailed statement of good cause with the appeal.
This is only considered under certain circumstances, such as if there is new evidence in the case or if an earlier decision was obviously wrong, or if dire circumstances prevented a timely filing.
Time limits for when an earlier application might be reopened for “good cause” after a missed deadline:
- SSDI has a four-year time limit
- SSI has a two-year time limit
h3 id=”h-when-all-appeals-are-exhausted”>When all Appeals Are Exhausted
A final denial means that you have exhausted all appeals or, in some cases, you missed a deadline.
If you receive a final denial, you may not reapply for SSDI under the same set of facts. This is because of a legal term called the doctrine of res judicata. This means you cannot litigate the same issue twice.
The SSA may use this doctrine
- to dismiss or refuse further action when a previous decision has been made and is final, or
- after a final decision is made, and no new facts or issues are presented to warrant a new case.
An example of presenting new information is when new evidence shows that a previous condition was more severe than it was originally thought, or when a period of disability has changed.
If you receive a final denial, you may still file a second application. In this case, you might allege the date you became disabled as the day after the ALJ decision. This establishes a different time period and thus bypass the doctrine of Res Judicata.
Chapter 7: The Administrative Law Judge (ALJ) Hearing
The most important level of appeal before the Social Security Administration is what is known as an ALJ Hearing. The hearing is informal and is conducted by an Administrative Law Judge (ALJ). The hearing takes place in the third step of the appeals process.
The hearings are usually conducted in a small conference room with the judge versus an official-looking courtroom. The hearing is recorded by a person known as a hearing monitor. All testimony is taken under oath, on penalty of perjury.
The hearing generally lasts about an hour to an hour and a half. It is seldom that these hearings take more than two hours.
h3 id=”h-the-administrative-law-judge-alj”>The Administrative Law Judge (ALJ)
An ALJ’s job is to issue an independent decision on your Social Security disability case. The decision should not be influenced by the fact your case was initially denied or reconsidered.
Fortunately, more than half of the ALJ decisions nationwide are in favor of the claimant.
h3 id=”h-informal-non-adversarial-hearing”>Informal Non-Adversarial Hearing
The ALJ hearing is a non-adversarial hearing, which means there is no lawyer on the other side who is going to ask you questions (or “cross-examine” you). The hearing is solely for a judge to find out the facts about your disability claim by asking you questions and/or calling other professionals to testify.
h3 id=”h-who-comes-to-the-hearing”>Who Comes to the Hearing
The ALJ hearing is a private hearing. While there is no attorney to cross-examine you in an ALJ hearing, you are allowed to choose whether you want an attorney or a non-attorney representative there to represent you.
In addition to the attorney or non-attorney representative, there are multiple professionals at the hearing that an ALJ may call to testify, including a vocation expert that can answer questions about job requirements, job availability and any hypothetical questions relating to your physical or mental limitations. A medical expert may also be called to testify.
Besides these officials and the hearing monitor, no other persons are able to attend the hearing without your permission.
h3 id=”h-what-questions-will-the-alj-ask”>What Questions Will the ALJ Ask?
An ALJ is interested in information about your disability. He or she will ask questions that center around the following topics: your work history; education; medical history; symptoms; estimated work limitations; and daily activities.
h3 id=”h-mental-limitations”>Mental Limitations
The issues of serious physical disabilities are sometimes worse after a long period of pain, which can add to your mental anguish. It is important to describe any emotional problems you might be feeling that interfere with or inhibit your ability to work, such as a difficulty concentrating; regular forgetfulness; nervousness; quick temper; non-social skills; crying spells; or depression.
Mental limitations might be the hardest to prove on paper, so an ALJ might ask you extensive questions regarding your ability to understand, carry out and remember instructions, make judgments, respond to supervisors or co-workers, or carry out routine work duties.
An ALJ may go as far as to ask you how well you deal with stress. If so, be clear on specific things or situations that you find stressful at work.
Below is an example of some situations that could lead to stress on a job:
- Meeting deadlines
- Completing job tasks
- Working with others
- Working with precision
- Completing complex tasks
- Making decisions
- Working within a schedule
- Facing criticism or taking instructions from supervisors
- Not knowing the chain of command
- The monotony of routine
- Getting to work regularly
- Anxiety about failing at work
h3 id=”h-what-a-lawyer-or-qualified-non-attorney-representative-does”>What a Lawyer or Qualified Non-Attorney Representative Does
Much of what your lawyer or non-attorney representative does to help your case is done outside the ALJ hearing. They gather medical evidence, get reports from doctors, do legal and medical research, prepare witnesses to testify and possibly make a closing argument either in writing or at the hearing.
While at the hearing, your representative might ask you to clarify information in your testimony that he or she thinks is not clear. He or she may also question any expert witnesses the ALJ calls to testify, as well as witnesses that you have opted to bring to the hearing.
Chapter 8: Developing Your Social Security Disability Case
The key to a disability claim is proving you are unable to perform any substantial gainful employment because of the disability you suffer.
Cases involving Social Security disability benefits are not designed to be adversarial. They are designed for you to prove you are not able to have any substantial gainful employment because of an impairment or disability.
The following describes important factors involved in building your case in hopes of winning your disability claim.
h3 id=”h-your-burden-to-prove-your-disability”>Your Burden to Prove Your Disability
The burden of proof, or the need to prove that you should qualify for Social Security disability benefits, lies on you, the claimant. That is why it is important to gather all medical information and any other evidence that will support the claim that you are disabled from working due to an impairment that will last for 12 months or longer.
h3 id=”h-evidence-used-to-determine-disability”>Evidence Used to Determine Disability
The following four elements of proof are weighed to determine if there is enough evidence to support a disability decision:
- Objective medical facts
- Diagnoses and opinions of your treating and examining physicians
- Your subjective evidence of pain
- Your educational background, age and work history
h3 id=”h-impact-of-your-treating-physicians-opinions”>Impact of Your Treating Physicians’ Opinions
SSA is to give treating physicians’ opinions great weight in determining disability. Likewise an ALJ must show good cause for rejecting the opinion of a treating physician who supports your disability case.
The ALJ must carefully and strongly weigh a treating physicians’ opinions, especially if they are well supported by medically accepted clinical and laboratory diagnostic techniques that are consistent with other substantial evidence in the case.
If the ALJ does reject the information, he or she must show good cause as to why.
h3 id=”h-duration-of-impairments”>Duration of Impairments
The period of duration of impairments is critical in determining whether you qualify for Social Security benefits. The durational requirement is satisfied when any one of the following occurs:
- The disability can be expected to result in death
- The disability has lasted continuously for at least 12 months
- The disability can be expected to last continually for at least 12 months
Chapter 9: The 5-Step Process for Proving You Are Disabled
The SSA disability evaluation system does not focus on your diagnosis. SSDI is based on the functional limitations you have. Your disability must be judged severe enough to prevent you from performing substantial gainful activity for 12 months or more.
When evaluating your disability claim, the SSA uses a five-step approach that considers your medical condition, ability to work, age, recent jobs, and education.
The process is commonly referred to as the Five-Step Sequential Evaluation.
h3 id=”h-the-five-step-sequential-evaluation”>The Five-Step Sequential Evaluation
Questions in the five-step inquiry are asked in a specific order. The questions are designed to be answered affirmatively or negatively in such a way that a decision can be made for or against the disability claim.
The burden of proof is yours at Steps 1—4.
At Step 5, the burden of proof shifts to the SSA adjudicator.
Listed are the questions in the Five-Step Evaluation and the answers that are necessary for each in order to be considered for Social Security disability benefits.
h3 id=”h-flow-chart-of-ssa-s-5-step-process-for-assessing-disability”>Flow Chart of SSA’s 5-Step Process for Assessing Disability

NOTE:
Step 1, a claim can be denied but not allowed.
Step 2, a claim can be denied but not allowed.
Step 3, a claim can be allowed but not denied.
Step 4, a claim can be denied but not allowed.
Step 5, a claim can be allowed or denied.
Here is another way to view the 5 Step assessment:
In order to qualify for Social Security disability, the following must be proved:
- You are not engaged in substantial gainful employment; and
- You have a severe impairment; and
- The impairment meets or equals one of the impairments described in the Social Security regulations known as the Listing of Impairments; or
- Considering your residual functional capacity (that is, what you can still do even with your impairments), you are unable to do past relevant work, and
- Other work within your residual functional capacity, considering your age, education and work experience, does not exist in the national economy in significant numbers.
You may learn more about SSA’s 5-Step evaluation at CFR § 404.1520 – Evaluation of disability in general.
Each of the five steps is explained below.
Chapter 10: Step One – You Are Not Gainfully Employed
No matter what your medical condition is, and regardless of your age, education and work experience, SSA will not grant a claimant disability benefits if he or she is gainfully employed. This is also referred to as performing Substantial Gainful Activity (SGA).
If SSA finds that you are not performing Substantial Gainful Activity, you move to step two of the Five Step Sequential Evaluation.
h3 id=”h-substantial-gainful-activity-sga”>Substantial Gainful Activity (SGA)
Substantial Gainful Activity is defined as work that requires significant physical or mental activities for pay or profit. It does not matter whether a profit is actually gained.
The level of income deemed to reach SGA status is different for blind and for non-blind claimants.
For example, for 2016, earnings exceeding $1,130 per month provide a rebuttable presumption that a non-blind claimant is engaging in SGA, while the amount for blind individuals is $1,820.
This presumption is rebuttable: meaning that while the SSA may assume that SGA has occurred, the non-blind claimant may contest it and prove otherwise. The burden is on the claimant to prove that
- he or she has not earned the amount paid, or
- he or she cannot sufficiently do the job (for which pay was earned) for long periods of time, or without special help.
h3 id=”h-self-employment-as-sga”>Self-Employment as SGA
If you are self-employed, SSA regulations hold that SGA encompasses your activities and their value, not just the incomed earned. Therefore, self-employment and seasonal work might be considered both substantial and gainful.
To illustrate this, one court opinion found a tax preparer’s seasonal business, which brought in under $1000 a year, was both substantial and gainful. In this case, the judge considered part time work to be substantial work.
h3 id=”h-part-time-work-as-sga”>Part-Time Work as SGA
While some part-time work places your income well below the annual threshold, such employment might still be considered substantial gainful activity.
For example: If you are disabled and work 25 hours a week and make $800 a month, you are well below the SGA limit. But suppose you also work (without pay) for 15 hours a week at the family store, running the cash register and doing other tasks. Although you are not paid wages for this work, the SSA may decide that you have the ability to perform at the SGA level. SSA may decide you are not disabled and therefore ineligible for benefits.
It is important to assert how a disability impacts you on a part-time job, especially if you are self-employed. In supporting documentation and at the ALJ hearing, explain how difficult it is to function in the part-time job, or how much help you need in order for you to do the job correctly.
If it takes a couple of days to recover from doing a part-time job, let the ALJ know that information.
h3 id=”h-illegal-activity-as-sga”>Illegal Activity as SGA
Illegal activity, such as drug dealing, prostitution or burglary can be regarded by Social Security as substantial gainful activity. It is also important to note that some illegal activity can disqualify you from receiving disability benefits if the benefits are ever awarded.
h3 id=”h-unsuccessful-work-attempts”>Unsuccessful Work Attempts
An unsuccessful work attempt is a work effort that lasts less than three months. This may happen because you can only do the work for a short period of time and then must stop due to your impairment, or because special conditions related to your impairment have been removed.
Your pay check stubs and other employment records are critical documentation that help to prove that your work history was sporadic. Be prepared to explain and prove that you are frequently unable to work and are counted as absent.
h3 id=”h-work-performed-under-special-conditions”>Work Performed Under Special Conditions
Various scenarios exist:
- Work done under special conditions, where you receive more assistance or oversight than is typically offered to other workers doing similar work, does not necessarily mean that you are performing Substantial Gainful Activity.
- If special conditions related to your condition and necessary to your work were removed, causing you to stop or limit work, SSA may decide that your work does not show that you are able to work at Substantial Gainful Activity.
- Alternatively, work performed under special conditions may show that you have the skills and ability to work at the SGA level.
Examples of the special conditions that may exist in your job include:
- Tasks that require you to receive specific assistance from co-workers in order to complete the work;
- Schedules allowing you to work variable or exclusive hours and take frequent breaks;
- Jobs that require you have special equipment, or tasks are assigned to you because they are particularly suited to your disabling condition;
- Instances where you are able to work only within a structure of specially arranged situations, such as where helpers enabled you to get ready to go to work, or travel to or from work;
- Tasks in which you are allowed to work at a lower standard of performance, skill or productivity than other employees;
- Opportunities where you are given the chance to work despite a disability—because of a family connection, past affiliation with the firm, or other charitable reason.
In addition, case law holds that an Administrative Law Judge has a duty to develop and process facts pertaining to the special conditions of your employment that arise from job coach assistance.
h3 id=”h-what-is-the-disability-onset-date-for-failed-work-attempts”>What Is the “Disability Onset Date” for Failed Work Attempts?
Failed work attempts do not count as work, so it is important that you document your disability date as the very first time your disability caused you to stop working.
Do not list your disability date as the last day you worked because doing so might prevent you from receiving several months of benefits to which you are entitled.
h3 id=”h-you-worked-more-than-three-months-but-less-than-six-months”>You Worked More than Three Months, but Less Than Six Months
If work was performed for more than three months, but less than six months, you must show additional evidence in order for the work to be considered an unsuccessful work attempt.
Some evidence to support the claim would be anything showing that
- there are frequent absences due to the impairment;
- the work was unsatisfactory due to the impairment;
- the work was done during a period of remission; or
- the work was done under special conditions.
Chapter 11: Step Two – Proving You Have a Severe Impairment
To qualify for SSDI, your impairment must be established as “severe” under Social Security rules. Proving a severe impairment is not easy. If SSA finds that your impairment or impairments are severe, then you continue to step three of the Five Step Sequential Evaluation.
Below is information regarding how SSA determines if your impairment is severe enough for you to receive Social Security disability benefits.
h3 id=”h-how-ssa-defines-severity”>How SSA Defines Severity
Severity in impairment occurs when an injury or illness—or combination of injuries or illnesses—notably interferes with your physical or mental ability to perform basic work activities.
Social Security disability benefits are not likely to be awarded if your health issues are considered slight. This is why it is important to have your treating physician specifically describe mental and physical limitations caused by a diagnosed condition.
For example, a doctor should write “the patient has difficulty with walking, standing, balancing and muscle control,” if that is the case, instead of using general terms like “the patient has difficulty performing duties at work.”
h3 id=”h-how-ssa-measures-severity”>How SSA Measures Severity
If your impairment is not deemed severe, then SSA will not consider you disabled. SSA does not factor in age, education and work experience. However, it is possible for you to have been disabled for a period of time in the past, even if a severe impairment no longer exists.
h3 id=”h-ssa-must-consider-the-combined-effects-of-all-of-your-impairments”>SSA Must Consider the Combined Effects of ALL of Your Impairments
Most people applying for disability benefits are dealing with more than one medical condition. An ALJ is charged with factoring in every impairment that you believe contributes to your inability to do basic work activities.
A combination of disabling conditions may be what it takes to raise your total classification from slight to severe, and thus meet the requirements of Step Two.
h3 id=”h-ssa-must-evaluate-your-subjective-symptoms-including-pain”>SSA Must Evaluate Your Subjective Symptoms, Including Pain
In addition to considering physical impairments, an ALJ must take into consideration subjective symptoms you endure, including pain. You need to build a strong case if a subjective symptom such as chronic pain is a major part of your condition.
Subjective symptoms are difficult to prove. Without a strong case in your favor, SSA has the opportunity to dismiss the allegation on exaggeration of symptoms.
If the alleged subjective symptoms can be accepted as consistent with the objective medical evidence and other evidence in the case record, then the symptoms could aid in the impairment being considered severe.
h3 id=”h-the-alj-s-duty-to-list-all-severe-impairments”>The ALJ’s Duty to List All “Severe” Impairments
In Step 2 of the evaluation process, the ALJ will discuss with you whether your impairment is severe. If your disability claim is based on more than one impairment, the ALJ has a duty to explain what impairment(s) are considered severe, and those considered not severe.
If the ALJ finds a minimum of one severe impairment, you move on to Step 3 of the Five Step Evaluation.
Chapter 12: Step Three – Proving Your Impairment Meets or Equals a Medical Listing
You may be found disabled without considering age, education and work experience
- if your impairment meets the duration requirement in the Social Security Act’s appendix (the inability to engage in SGA due to an impairment that must last the required 12-month period) – OR –
- if you have a condition that is equal to a listed impairment.
If SSA finds that your impairment(s) meets either of the above requirements, you would be found disabled and you are eligible for benefits.
Otherwise, you must move on to prove your claim under Step 4 of the Five Step Sequential Evaluation.
h3 id=”h-what-is-a-ssa-medical-listing”>What Is a SSA Medical Listing?
Medical conditions including mental disorders are evaluated by specific rules. These rules are published in the SSA Listing of Impairments. The SSA Listings describe all medical conditions that qualify for automatic approval, once proved.
h3 id=”h-ssa-uses-medical-expert-opinions”>SSA Uses Medical Expert Opinions
The SSA has the right to rely on the opinions of reviewing physicians when assessing if you meet requirements of the listing.
h3 id=”h-proving-you-meet-a-medical-listing”>Proving You Meet a Medical Listing
You bear the burden of proving that your impairment(s) meets or equals a listed impairment. Therefore, you must satisfy all the criteria of the listed impairment.
Example: If a spine disorder has rendered you unable to work, the SSA will review all medical evidence, including treatment regimens and hospitalization, to determine if your impairment meets the requirements or is equal in severity to what is stated in the SSA listing for disorders of the spine.
h3 id=”h-proving-you-equal-a-medical-listing”>Proving You Equal a Medical Listing
You may have a medical condition that does not completely meet the criteria of an SSA listing. Still, your condition may be medically equivalent to a listed impairment.
In this case you must prove that your condition disables you just as much as someone with a disorder that meets the listing. The claim must be extensively supported with medical evidence and doctor’s opinions, with arguments proving functional limitations, to substantiate and demonstrate equivalence.
If SSA finds that your condition is medically equal in severity and duration to a listed impairment, your condition will be considered medically equivalent to the listing, and you would be eligible for benefits.
h3 id=”h-the-alj-s-duty-in-medical-impairment-s”>The ALJ’s Duty in Medical Impairment(s)
If your medical impairment does not meet or equal a listing, it is the ALJ’s obligation to explain the reason(s) why and discuss the evidence with you. The ALJ cannot simply summarize that your impairments do not meet or equal any listing.
h3 id=”h-ssa-listing-categories”>SSA Listing Categories
A free, listing of impairments is found at ssa.gov.
Categories include:
1.00 – Musculoskeletal System
2.00 – Special Senses and Speech
3.00 – Respiratory System
4.00 – Cardiovascular System
5.00 – Digestive System
6.00 – Genitourinary Disorders
7.00 – Hematological Disorders
8.00 – Skin Disorders
9.00 – Endocrine Disorders
10.00 – Congenital Disorders that Affect Multiple Body Systems
11.00 – Neurological
12.00 – Mental Disorders
13.00 – Cancer (malignant neoplastic diseases)
14.00 – Immune System Disorders
Chapter 13: Residual Functional Capacity (RFC)
Before moving on to Steps Four and Five of the evaluation, learn why Residual Functional Capacity (RFC) is often the most critical part of your claim during this stage of the process.
Steps 4 and 5 are:
- Step 4: Can You Perform Past Relevant Work?
- Step 5: Can You Perform Other Available Work?
In these steps, all medical and non-medical evidence will be considered, including medical records, observations by examining physicians, evaluations of the medical evidence by non-examining physicians, and the testimony of the claimant and others who have observed the claimant.
h3 id=”h-what-is-rfc”>What is RFC?
RFC is an evaluation of your capacity for full-time work. It defines the activities you can still do regardless of your physical or mental impairments. Your RFC is the maximum remaining ability you have to do work activities in an ordinary work setting on a “regular and continuing basis.”
A regular and continuing basis means work done for eight hours a day for five days a week, or an equivalent schedule. Your RFC is expressed in terms of the exertional (strength) classifications of work.
There are five exertional RFC levels of work:
- sedentary
- light
- medium
- heavy
- very heavy
h3 id=”h-rfc-exertional-strength-activities-described”>RFC: Exertional (Strength) Activities Described
There are seven primary strength, or “exertional,” activities of work used in understanding your RFC.
Exertional activities are centered on three work positions
- sitting
- standing
- walking
and four worker movements of objects
- lifting
- carrying
- pushing
- pulling
h3 id=”h-exertional-rfc-level-standards”>Exertional RFC Level Standards
The five exertional RFC levels of work activity are: sedentary, light, medium, heavy and very heavy work.
Each exertional level is then defined in terms of the degree that the seven primary strength demands of jobs are required.
Sedentary Work
- Sitting should generally total about six hours of an eight-hour workday
- Periods of standing or walking should generally total no more than two hours of an eight-hour workday
- Lifting no more than 10 pounds at a time
- Occasionally lifting or carrying articles like docket files, ledgers and small tools
- The term “occasionally” means occurring from very little up to one-third of the time
Light Work
- Requires standing or walking off and on for a total of about six hours in an eight-hour workday
- May involve sitting most of the time, but with some pushing and pulling of arm-hand or leg-foot controls that require greater exertion than in sedentary work
- Lifting no more than 20 pounds at a time
- Frequent lifting or carrying of objects weighing up to 10 pounds
- “Frequent” means occurring from one-third to two-thirds of the time
- If you can do light work, SSA determines you can also do sedentary work, unless there are additional limiting factors such as loss of fine dexterity or inability to sit for long periods.
Medium Work
- Requires standing or walking off and on, for a total of about six hours in an eight-year workday
- As in light work, sitting may occur intermittently during the remaining time
- Lifting no more than 50 pounds at a time
- Frequent lifting or carrying of objects weighing up to 25 pounds
- “Frequent” here means occurring from one-third to two-thirds of the time
- If you can do medium work, SSA determines you can also do light and sedentary work.
Heavy Work
- Requires standing or walking off and on, for a total of about six hours in an eight-hour workday
- Lifting objects weighing no more than 100 pounds at a time
- Frequent lifting or carrying of objects weighing up to 50 pounds
- If you can do heavy work, SSA determines that you can also do medium, light and sedentary work.
Very Heavy Work
- Requires standing or walking off and on, for a total of about six hours in an eight-hour workday
- Lifting objects weighing more than 100 pounds at a time
- Frequent lifting or carrying of objects weighing 50 pounds or more
- If you can do very heavy work, SSA determines that you can also do heavy, medium, light and sedentary work.
h3 id=”h-how-rfc-is-impacted-by-the-sit-stand-option”>How RFC is Impacted by the Sit/Stand Option
SSA rules hold that a person who may be able to sit for a time, but must then get up and stand and walk awhile before sitting again, is therefore not functionally able to perform either the extended sitting considered in the definition of sedentary work, or the extended standing or walking considered for most light work.
h3 id=”h-rfc-consideration-of-all-physical-and-mental-impairments”>RFC: Consideration of ALL Physical and Mental Impairments
In reaching a decision of RFC, and having assessed your medical impairments, the ALJ must establish the physical and mental activities that you can perform in a work setting as based on medical evidence, and any impairments (including pain) that affect physical and mental activities.
h3 id=”h-rfc-effect-of-mental-impairments”>RFC: Effect of Mental Impairments
The ALJ determines how mental impairments asserted in your claim further limit any exertional tasks that you are regarded capable of handling.
The evaluation of RFC in claims alleging mental disorders includes consideration of the ability to understand, to execute and remember instructions, and to respond appropriately to supervision, coworkers and typical work pressure in a work setting.
To make this RFC determination, an ALJ considers the following evidence:
- Detailed medical records including all findings and opinions of your treating psychiatrist or psychologist and other mental health specialists.
- Reports of your activities of daily living and work activity; this may include testimony of others regarding your performance behavior.
- Assessment of the quality of your daily activities in work and social environments.
- Are you able to sustain activities and interests, and do you relate to others over a period of time? The ALJ will also look into how frequent and how appropriate your activities are.
- At what level are you able to function intellectually?
- What is your ability to function in a work-like situation?
h3 id=”h-rfc-consider-non-medical-evidence”>RFC: Consider Non-Medical Evidence
Subjective reports of pain and workplace performance can help assess RFC. Input from sources including social workers and family members can be vital to your case.
This might include performance and functional limitation in any type of work setting. Non-medical evidence can be influential in assessing the person’s ability to function in a competitive work environment.
h3 id=”h-the-record-must-support-the-rfc”>The Record Must Support the RFC
An ALJ’s closing statements must specify the functions that you are still capable of doing. The RFC can only be determined when there is substantial evidence of each physical requirement listed in the regulations.
h3 id=”h-absenteeism-how-it-affects-the-ability-to-work”>Absenteeism: How it Affects the Ability to Work
You are entitled to have a vocational expert evaluate your disability-related excessive absenteeism, particularly when you would be absent from the workplace an extreme amount of time due to physical or mental impairments, or due to treatment regiments for such impairments.
Chapter 14: Step Four – Proving You Can’t Do Your Past Relevant Work
The SSA will find that you are not disabled if your impairment does not prevent you from being able to perform any of your past relevant work.
Past relevant work is generally defined as full-time work that meets the following criteria:
- You performed the work in the past 15 years
- The work lasted long enough for you to learn to do it (reach average performance)
- The work was substantial gainful activity
When the SSA cannot make a decision based on your current work activity and medical facts alone, and it is established that you have severe impairments, RFC plays an important role.
h3 id=”h-your-burden-to-establish-an-inability-to-perform-past-relevant-work”>Your Burden to Establish an Inability to Perform Past Relevant Work
You have the initial burden of proving disability by establishing a physical or mental impairment that lasts at least 12 month and prevents you from engaging in any work. You maintain this burden of proof for the first four steps in the five-step sequential evaluation.
At this step SSA does not consider your age, education, employability, or whether past relevant work exists in significant numbers in the national economy.
The fifth step is when the burden shifts to the SSA to show if you can perform other work.
h3 id=”h-alj-considers-rfc-physical-and-mental-requirements-of-past-work”>ALJ Considers RFC & Physical and Mental Requirements of Past Work
The ALJ will review your RFC and physical and mental requirements of your past jobs in order to decide whether you can do work you did in the past.
To do so, the SSA and most vocational experts use the Dictionary of Occupational Titles (DOT) to determine the RFC requirements and skill level of past jobs. Published by the Department of Labor, the DOT lists thousands of jobs and their requirements, including their strength and skill levels.
Mental RFC is evaluated according to mental demands of work as described in the Code of Federal Regulations (CFR).
It is especially important in mental claims of disability that you specifically list which job duties produce the onset of conditions such as tension and anxiety. Cases have been denied in the past because of a lack of description.
h3 id=”h-short-work-periods”>Short Work Periods
Work performed for a short period of time is not considered relevant.
h3 id=”h-work-performed-more-than-15-years-ago”>Work Performed More Than 15 Years Ago
The regulations provide that it is not realistic to expect that skills and abilities acquired in a job done more than 15 years ago still apply. Therefore, only work you performed within the 15-year period prior to the adjudication (or formal judgement on a disputed matter) should be considered in determining past relevant work.
You will have to prove that you can no longer do each of the jobs you list. You need to be honest, but be sure to avoid listing jobs that you did not work long enough to learn, such as short-term and part-time jobs.
h3 id=”h-work-that-is-unavailable”>Work that is Unavailable
SSA assumes that if you can still perform the physical and mental requirements of a previous job, you are functionally able to do that work. This is true even if you no longer live in the country where you performed that work.
When this is the case, you may be denied disability benefits.
It is still up to you in step four of the five-step sequential evaluation process to prove your disability. Only in the fifth step does the burden shift to the SSA to determine whether work that you can perform is available in the national economy.
h3 id=”h-a-vocational-expert-is-not-needed-at-step-four”>A Vocational Expert is Not Needed at Step Four
A vocational expert is not needed to determine whether you can perform your past work. A vocational expert is actually not necessary until the fifth step of the sequential evaluation process, when the burden of proof shifts to the SSA to prove that jobs exist that you can perform.
h3 id=”h-past-relevant-work-needs-to-be-considered-substantial-gainful-activity”>Past Relevant Work Needs to be Considered Substantial Gainful Activity
Past relevant work covers all previous work that rises to the level of substantial gainful activity. If you can do past work when work experience reaches the SGA level, it may indicate you are still capable of engaging in SGA.
If you show that your impairment prevents you from being able to do past relevant work, you now proceed to Step 5.
Chapter 15: Step Five – Proving You Cannot Do Any “Other Work”
If you are claiming to be disabled, not only should your impairment disable you from doing past work, but it should prevent you from doing any other work.
SSA therefore considers your residual functional capacity, age, education and past work experience to see if there is any work that can be done. If not, SSA will find you disabled.
h3 id=”h-it-is-ssa-s-burden-to-establish-your-ability-to-perform-other-work”>It Is SSA’s Burden to Establish Your Ability to Perform Other Work
The final step in the five-step sequential evaluation process requires the SSA to prove if there are other jobs you can do. SSA usually does this with the help of a vocational expert.
If you can make an adjustment to other work, you will be found to be not disabled.
If you cannot adjust to other work, you will be found to be disabled.
Representation by an experienced attorney or non-attorney representative is essential in this process in order to cross-examine the vocational expert when necessary. Remember, you do not have to prove anything in this step, but you do have the right to question any information they provide that is contrary to your abilities.
h3 id=”h-use-of-the-medical-vocational-guidelines-grid-rules-to-determine-disability”>Use of the Medical-Vocational Guidelines (Grid Rules) to Determine Disability
SSA resorts to a “grid” (5-column table) of rules that outlines criteria under which a person is deemed disabled. The criteria is based more on vocational facts and realities and less on medical impairments. The criteria include residual functional capacity, age, education and past work history.
The grid rules give the SSA a uniform method for finding a person disabled even if he or she can still do some level of work.
h3 id=”h-using-the-grid-rules-to-direct-a-finding-of-disabled-or-not-disabled”>Using the Grid Rules to Direct a Finding of “Disabled” or “Not Disabled”
The SSA will make a determination of disabled or not disabled by assessing your
- RFC
- age
- education
- previous work experience.
Note, the use of Medical-Vocational guidelines, or grid rules, is warranted only when impairments are considered exertional — they must only be physical limitations, and not mental or emotional disorders.
If you do not have mental or emotional impairments, then the grid rules will direct the SSA in making a determination of disability.
h3 id=”h-how-your-age-affects-the-application-of-the-grids”>How Your Age Affects the Application of the Grids
SSA realizes that as people age they have a harder time finding employment. Older age is an increasingly negative vocational factor for persons with severe impairments.
In short, the standard by which you can be found disabled by SSA gets easier the older you get. Ages 45, 50, 55 and 60 are critical ages to a decision.
Some borderline situations may happen in which the chronological ages do not apply, such as if you were on the borderline closer to one age than another (for example, if you are 54 years and 11 months you might be classified within the advanced age of 55).
Four “age” categories govern the grid rules:
Younger Individual (under age 50)
- Ages 45-49
- Ages 18-44
Closely Approaching Advanced Age
- Ages 50 through 54
Advanced Age
- Ages 55 through 59
Closely Approaching Retirement Age
- Ages 60 through 64
h3 id=”h-education-and-illiteracy-in-the-grids”>Education and Illiteracy in the Grids
In addition to the effect of age on the grid rules, there are six “education” categories underlying the grid rules.
- Inability to Communicate in English
SSA may consider speaking, reading, communicating or understanding English as an educational factor for multiple reasons. For example, it may be difficult for someone who doesn’t speak and understand English to do a job, regardless of the amount of education obtained in another language. - Illiteracy
This is the inability to read or write. If a person cannot read or write a simple message, such as instructions or inventory lists, it may be determined that the person has had little or no formal schooling, even if the person is able to sign his or her name. - Marginal Education
A person with marginal education has the ability in reasoning, arithmetic and language needed to do simple, unskilled types of jobs. SSA generally considers formal schooling to be at a sixth grade level or less. - Limited Education
A person with limited education has abilities in reasoning, arithmetic and language skills, but does not have enough education or ability to allow that person to do most of the more complex job duties needed in semi-skilled or skilled jobs.SSA generally considers an education from the seventh through 11th grade levels of formal education as a limited education. - High School Graduate and Above (Does Not Provide for Direct Entry into Skilled Work)
The SSA considers a high school education or more as abilities in reasoning, arithmetic and language skills acquired through formal schooling at a 12th grade level or higher.As a general rule, SSA views someone with these educational abilities as able do semi-skilled through skilled work. The criterion of a high school or higher education provides for direct entry into skilled work, especially when there is little time lapse between the completion of formal education and the date of adjudication. - High School Graduate or More (Does Provide for Direct Entry into Skilled Work)
High school education and above means abilities in reasoning, arithmetic and language skills acquired through formal schooling at a 12th grade level or above. SSA generally considers that someone with these educational abilities can do semi-skilled through skilled work.
h3 id=”h-job-skill-levels-in-the-grids”>Job Skill Levels in the Grids
Work experience in the grids is expressed in terms of skill level. There are three categories of job skill levels:
- Unskilled
Unskilled work consists of simple duties that can be learned on the job in a short period of time, and where little or no judgment is needed to perform the tasks. The job may or may not require considerable strength.A job is typically unskilled if it can be learned in less than 30 days and there is little specific vocational preparation or judgment needed. A person does not gain work skills by doing unskilled work. - Semiskilled
Semiskilled work requires some skills, but not enough that would be required for more complex work duties.Semiskilled jobs may require alertness and close attention to watching machine processes or inspecting, testing or guarding equipment. Semiskilled jobs may require dexterity and coordination, such as moving your hands or feet quickly to perform repetitive tasks. - Skilled
Skilled work calls for a person to use judgment to determine the machine and manual operations to be carried out in order to obtain the proper form, quality or quantity of material to be produced.Skilled jobs may demand design and planning work, estimating quality, determining the suitability and needed volume of materials, making exact measurements, reading blueprints or other specifications, or making necessary calculations or mechanical adjustments to administer and manage the work.Other skilled employment may involve dealing with people, facts or figures or abstract ideas on a highly complex level.
h3 id=”h-loss-of-hands-and-finger-use-and-your-ability-to-perform-unskilled-sedentary-work”>Loss of Hands and Finger Use and Your Ability to Perform Unskilled, Sedentary Work
Most unskilled sedentary jobs require good use of the hands and fingers for repetitive hand-finger actions. If impairments prevent the use of your hands, fingers and/or arms for repetitive hand-finger actions, and if you are performing limited to unskilled, sedentary work, the job base may be so eroded for you that you may be found unemployable.
h3 id=”h-past-work-experience-are-your-skills-transferable”>Past Work Experience: Are Your Skills Transferable?
SSA may assess past work experience as: 1) none, 2) not vocationally relevant, 3) unskilled, 4) semiskilled, or 5) skilled.
Skilled or semiskilled job experience is usually transferable to another job and above the unskilled level of complexity. These skills must be identifiable and must be able to be used in specific skilled or semiskilled occupations within your RFC.
h3 id=”h-vocational-expert-testimony-is-used-when-grids-are-not-applied”>Vocational Expert Testimony Is Used When Grids Are Not Applied
Your case may not warrant the use of Grid Rules in making a decision. If that is the case, SSA may only sustain its burden of proof by producing expert vocational testimony concerning the existence and availability of jobs in the national economy in which you can perform.
h3 id=”h-job-availability-in-the-national-economy”>Job Availability in the National Economy
For the SSA to decide that you can perform other work, the work must be readily available in significant numbers in the national economy.
h3 id=”h-structure-of-the-medical-vocational-guidelines-grids”>Structure of the Medical-Vocational Guidelines (Grids)
Due to the column-and-row structure, the medical-vocational guidelines are known as “the grids.”
At step five of the sequential evaluation, the grids show SSA’s analysis of the impact of the statutory vocational factors of disability, which are
- age
- education
- previous work experience
The grid rules combine these vocational factors with the medical factor (residual functional capacity (RFC)) on your ability to perform other work.
Each medical-vocational rule within a grid table is comprised of two elements:
- A medical profile, i.e. an exertional RFC (sedentary, light or medium)
- A vocational profile (age, education and previous work experience)
The grid rules resolve the Step Five issue—are you able to perform other available work?—by taking administrative notice of the fact that,
- given your sedentary, light, or medium RFC, and
- considering your age, education and work experience
you can or cannot engage in work that exists in significant numbers in the national economy.
If your medical-vocational profile (RFC, age, education and previous work experience) matches one of the grid rules, that grid rule conclusively determines whether the statutory definition of disability is satisfied.
For instance, when your medical-vocational profile matches that of a grid rule, that grid rule establishes an irrefutable presumption that you are either disabled or not disabled, and the particular grid rule must be used in making a determination. Where a grid rule directs a finding of disabled, vocational expert testimony may not rebut the conclusion directed by the grid rule.
The grids consist of tables of rules which are based on the full range of the five physical exertional RFC levels – sedentary, light, medium, heavy and very heavy.
The RFC component of the tables incorporates the medical element of the definition of disability. Of the 82 numbered grid rules in the medical-vocational tables, only 17 rules direct a finding of disabled.
h3 id=”h-the-grids-maximum-rfc-permitted-for-disability-finding”>The Grids: Maximum RFC Permitted for Disability Finding
| Age | Education | Previous work experience | Max. RFC | Rule |
| 60-64 | 6th grade or less | Unskilled | Medium | 203.01 |
| 7th to 11th grade | Unskilled | Light | 202.01 | |
| 11th grade or less | None | Medium | 203.02 | |
| 11th grade or less | Skilled/semiskilled. Skills not transferable | Light | 202.02 | |
| High school grad or more. Does not provide for direct entry into skilled work | Unskilled or none | Light | 202.04 | |
| High School grad or more. Does not provide for direct entry into skilled work | Skilled/semiskilled. Skills not transferable | Light | 202.06 | |
| 55-59 | 11th grade or less | None | Medium | 203.10 |
| 11th grade or less | Unskilled | Light | 202.01 | |
| 11th grade or less | Skilled/semiskilled. Skill not transferable | Light | 202.02 | |
| High school graduate or more does not provide for direct entry into skilled work | Unskilled or none | Light | 202.04 | |
| High school graduate or more does not provide for direct entry into skilled work | Skilled or semiskilled. Skills not transferable | Light | 202.06 | |
| 50-54 | Illiterate or unable to communicate in English | Unskilled or none | Light | 202.09 |
| 11th grade or less – at least literate and able to communication in English | Unskilled or none | Sedentary | 201.09 | |
| High school graduate or more, does not provide for direct entry into skilled work | Unskilled or none | Sedentary | 201.12 | |
| High school graduate or more does not provide for direct entry into skilled work | skilled/semiskilled Skills not transferrable | Sedentary | 201.14 | |
| 45-49 | Illiterate or unable to communicate in English | Unskilled or none | Sedentary | 201.17 |
| All education levels, Literate and able to communicate in English | Unskilled, none, or skilled or semiskilled – skills not transferable | Sedentary occupational base must be significantly eroded. | 201.00(h) | |
| 18-44 | All educational levels including illiterate or unable to communicate in English | Unskilled, none, or skilled or semiskilled – skills not transferable | Sedentary occupational base must be significantly eroded. | 201.00(h) |
h3 id=”h-grids-as-a-framework-for-decision-making”>Grids as a Framework for Decision Making
Your exertional RFC may differ from the SSA definitions of sedentary, light or medium work on which the medical–vocational tables are based. For example, if your RFC for exertional activity is somewhere between sedentary and light work—then you have exertional limitations that are not described by the grids.
In this case, the grids are used only as a framework for decision making. They do not direct a finding of disabled or not disabled.
If your condition limits your ability to work without directly affecting your exertional abilities, you are said to have a non-exertional limitation.
Non-exertional limitations include impairments that are mental, sensory, postural, manipulative or environmental (such as the inability to tolerate dust or fumes). In these cases as well, the grids do not fully apply and are used only as a framework for decision making.
h3 id=”h-rfc-for-less-than-a-full-range-of-sedentary-work”>RFC for Less Than a Full Range of Sedentary Work
Under the grid rules, claimants under age 50 must be able to do much less than a full or wide range of sedentary work and must not be able to do jobs that are available in significant numbers for claimants under age 50.
This is called “significant compromise of the sedentary occupational base.”
While it is difficult to show this, it is not impossible. Common impairments used to prove the inability to perform at the sedentary level include the following:
- The inability to stand or walk more than two hours per day
- Side effects of medication
- Inability to lift and carry 10 pounds for one-third of an eight-hour day
- The need for frequent unscheduled breaks
- High absenteeism
If you are under age 50, it is necessary to show that you cannot do sedentary or light work because it shows that surely you are unable to do medium or heavy work.
To accomplish the difficult issue of proving this you will usually look for a combination of exertional and nonexertional impairments.
Each additional impairment whittles away the range of sedentary work that you are capable of doing to arrive at the point where jobs do not exist in significant numbers.
h3 id=”h-nonexertional-limitations”>Nonexertional Limitations
While exertional abilities involve sitting, standing, walking, lifting, carrying, pushing and pulling, any other work-related ability is called a nonexertional limitation. A list of categories and examples is as follows:
| Category | Example |
| Postural | Need to alternate sitting or standing or to elevate leg(s) Difficulty turning head Balance problems or difficulty bending, stooping or squatting Use of a cane or walker |
| Manipulative | Difficulties reaching, grasping, handling or fingering |
| Environmental | Difficulties working around fumes, dust, etc. Difficulties tolerating noise, heights, humidity or temperatures Inability to be around dangerous machinery |
| Mental | Difficulties relating with others Not understanding, remembering or following basis instructions Inability to maintain attention, concentration, pace or accuracy Poor stress tolerance |
| Sensory | Difficulties speaking, hearing, feeling or seeing |
| Pain | Effects of cognitive abilities as described in mental category |
The above list is by no means an all-inclusive list of nonexertional impairments. Many impairments have both exertional and nonexertional implications.
For example, amputation of an arm will limit the weight you can lift (which is exertional) and will also limit bimanual dexterity (which is nonexertional). Vocational expert testimony is often necessary for evaluating the impact of such limitations.
h3 id=”h-work-skills-that-can-transfer-to-another-job”>Work Skills that can Transfer to Another Job
The Medical-Vocational Guidelines indicate that a claimant is never disabled if he or she has work skills that are transferable to jobs within his or her RFC and exist in significant numbers.
A finding of no transferable work skills may lead to a finding of disability in cases where you otherwise meet the grid listing.
It is important not to overstate job titles, training or education because of the complicated issue of transferrable skills. The more skills the SSA thinks you have, the harder it is to show you have no transferable skills.
If you are age 50 or older and are limited to sedentary work, you win or lose the case based upon whether you have skills transferable to sedentary work. If you are age 55 or older, this rule extends to light work, as well.
Chapter 16: Getting Help with Your SSDI Claim
Social Security law is highly complex. The very complexity of the process is the reason why most individuals who apply are denied.
Having the right help with your Social Security disability claim can make the difference in winning or losing benefits, and in how quickly you may qualify for benefits.
You have the right to appoint a qualified individual to represent you in your claim for Social Security Disability benefits. The appointment must be in writing and filed with SSA.
Your SSDI representative must be an attorney or a qualified non-attorney representative.
h3 id=”h-attorney-vs-non-attorney-representation”>Attorney vs. Non-Attorney Representation
Attorney Representation
A disability attorney is able to advise you on the law and can interpret the law to build a case that avoids the pitfalls that cause so many SSDI claims to be denied in the first place. A lawyer who focuses on Social Security Disability benefits, or is Board Certified in Social Security disability law, takes out the guess work in your disability case.
Non-attorney Representation
SSA requires that non-attorney representatives possess a bachelor’s degree or equivalent qualifications, pass SSA’s written examination, secure professional liability insurance or equivalent, undergo a criminal background check, and complete continuing education courses.
It is important to know the qualifications of a non-attorney representative who wants to represent you during your Social Security disability claim. Some non-attorney representatives may have experience as former SSA claims examiners, field workers and ALJs and thus are familiar with the disability claim process.
There are various organizations that allege that they can represent you, but there are some factors to consider beforehand.
Example 1:
A non-attorney representative cannot represent you in federal court, should your case rise to that level. Their ability ends with answering questions concerning Administrative policies and procedures.
Example 2:
You may also have a long term disability (LTD) claim going on at the same time as your SSDI claim. LTD insurance companies team up with non-attorney advocates. Be aware if your insurance company recommends using a Social Security Disability “firm” to help you get SSDI benefits. Their purpose is to win your case and collect your back due benefits to reimburse your insurance company.
Example 3:
The cost for both a lawyer and a non-lawyer representative is the same because fees are strictly regulated the SSA.
- Both attorneys and non-attorneys are paid 25% of back benefits, capped at $6000.
- Both attorneys and non-attorneys must work on contingency, which means you pay them only if they win your case.
The following table further explains attorney vs. non-attorney representation.
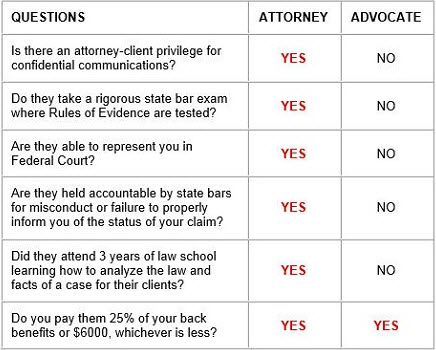
It is up to you and your disability lawyer or non-attorney advocate to develop the facts of your case, research the law, and frame issues for courts to decide in your favor.
h3 id=”h-what-will-a-qualified-ssdi-attorney-do-for-me”>What Will a Qualified SSDI Attorney Do For Me?
Each disability case is different. Generally, an experienced attorney does the following things to assist in a Social Security Disability claim:
- Aids you in filling out all SSA forms
- Evaluates your claim and advises you on the law and your options
- Reviews your medical records and makes suggestions for any additional testing required to prove your case
- Supplements your claim file with additional medical records
- Files any appeals necessary and handles all SSA paperwork
- Obtains medical reports and opinion evidence regarding your disability
- Consults with qualified vocational experts to get opinion evidence rebutting the ALJ-called vocational experts
- Obtains and develops evidence regarding your Residual Functional Capacity, which is the key to your disability claim
- Correctly calculates your benefits
- Files a legal brief arguing the legal, medical and vocational issues in your case
- Files a lawsuit in federal court if necessary
- Files your Motion for Summary Judgment and responds to the government’s Motion for Summary Judgment filed against you
h3 id=”h-what-will-an-ssd-advocate-non-attorney-do-for-me”>What Will an SSD Advocate (Non-attorney) Do For Me?
An SSDI advocate who is not a lawyer can also do many things to ensure that an SSDI or SSI claim is developed in a way to receive a favorable decision.
As with a disability attorney, your SSD Advocate will research and assemble your medical records; aid you in completing all SSA forms and evaluate your claim. He or she cannot offer you legal advice. Neither can he or she appeal your case to the federal level, should that become necessary.
h3 id=”h-expenses-are-the-same-for-attorney-and-non-attorney-representatives”>Expenses Are the Same for Attorney and Non-Attorney Representatives
Social Security regulations allow you to hire a representative on a contingent fee basis, which means you will not have to pay any fees up front to be represented by an attorney or a non-attorney representative for your claim.
If you win your disability case, your legal or non-legal team is entitled to 25 percent of all past benefits up to a maximum of $6,000 if the case is won before appealing to the federal district court.
Only an attorney may represent a case to federal court. If your case must be appealed to federal district court, the $6,000 maximum cap is lifted and the attorney fee is up to 25 percent of all past due benefits.
Note: Although an SSDI representative’s fee is not charged up front, other charges typically occur as your disability claim is prepared. Many states laws require free medical records for SSDI claimants, but this does not necessarily apply to out-of-state medical records. It may also cost money to obtain your file from SSA. Doctors frequently charge a fee to fill out medical questionnaires.
h3 id=”h-where-to-find-an-ssd-attorney-or-non-attorney-advocate”>Where to Find an SSD Attorney or Non-Attorney Advocate
You can find qualified SSDI attorneys and non-lawyer representatives by various means, including
- Your state bar association, or local legal aid offices
- The National Organization of Social Security Claims Representatives (NOSSCR) operates a national referral service for its members. You can visit NOSSCR.org for more information.
- The National Board of Trial Advocacy also has a website that can assist you in finding attorneys who are Board Certified in Social Security Disability Law, by state or alphabetically in the United States.
- Internet search and yellow pages
- Your local SSA office may assist with locating local bar associations and legal aid services
There is no guarantee that you have a better chance of winning a case with an attorney or a non-attorney representative. However, hands-on help from an experienced lawyer or non-attorney rep can be the deciding factor in having your case properly developed to prevail against any challenge presented by an SSA examiner or judge, and at the earliest stages.
Chapter 17: Winning Social Security Disability: What Happens Next?
The following section answers questions that most people have after receiving a favorable Social Security disability decision. The answers are general, so consult with a knowledgeable attorney or non-attorney representative about your specific situation.
h3 id=”h-do-i-have-to-do-anything-in-order-to-receive-my-payments”>Do I have to do anything in order to receive my payments?
Benefit payments after a favorable Social Security disability decision are automatic. You will not have to make a trip to the Social Security office or fill out forms in order to get paid.
However, if you have children who were under age 18 (or under age 19 and still in high school) at any time after your “date of entitlement,” you will need to put in an application for them to receive benefits.
h3 id=”h-when-will-ssa-start-paying-me”>When will SSA start paying me?
If you did not apply for SSI, it usually takes one to two months for back benefits to be paid and for monthly Social Security disability benefits to begin.
When SSI is involved it takes considerably longer. In some cases, it takes as long as three months for back Social Security disability benefits to be paid.
If it takes more than 90 days for back benefits to be paid, you should investigate your case for any problems by going to your local SSA field office.
h3 id=”h-how-far-back-will-ssa-pay-me-benefits”>How far back will SSA pay me benefits?
Your disability payments will begin after the expiration of the full, five-month waiting period from your date of entitlement. This is generally the date SSA determined you became disabled.
Another rule limits payment of back benefits to 12 months before the date of the application. Therefore, your benefits begin either 12 months before the date of application or five full months after the date you were found to be disabled, whichever is later.
h3 id=”h-what-will-the-amount-of-my-monthly-check-be”>What will the amount of my monthly check be?
The Payment Center will contact you regarding the monthly amount, but it is possible that SSA recalculates your benefit amount before paying you. If this happens, SSA may come up with a higher benefit amount for multiple reasons, such as if all your earnings might not have been posted when the original calculation was made.
There are also cost of living increases that are considered and/or applied every December.
h3 id=”h-will-i-receive-a-notice-from-ssa-explaining-my-benefits”>Will I receive a notice from SSA explaining my benefits?
You usually will receive what is called the “Notice of Award,” which shows you the date of entitlement, the amount of benefits per month, and back benefits to which you are entitled.
The notice will also show the amount of benefits withheld for direct payment of fees for an attorney or a non-attorney representative.
It may also give information about your Medicare eligibility and monthly Medicare premium. In addition, there may be some information provided about when to expect a “continuing disability review.”
h3 id=”h-when-will-the-notice-of-award-come-in-the-mail”>When will the Notice of Award come in the mail?
The Notice of Award will come around the time (usually afterward) that you receive your check for past due benefits.
h3 id=”h-should-i-wait-until-i-receive-the-notice-of-award-before-i-cash-my-check-for-past-due-benefits”>Should I wait until I receive the Notice of Award before I cash my check for past due benefits?
There is no need to wait to cash a Social Security disability benefits check.
It is generally a good idea to deposit your check into an interest bearing savings account and not spending all of it until you receive the Notice of Award. That way, you will know for sure that attorney’s fees were withheld and that you have not been overpaid.
It is also a good idea to make two photocopies of the check before you deposit it and to send one copy to the attorney while retaining the other copy for your records.
h3 id=”h-why-would-there-be-a-problem-if-i-was-overpaid”>Why would there be a problem if I was overpaid?
SSA almost always figures out whether someone has been paid too much, and SSA always finds a way to collect the overpayment. If you do not have the money to repay the full amount of the overpayment, SSA may threaten to cut off your checks until the overpayment is recouped.
However, SSA will usually accept a more reasonable reduction of your monthly checks, which can still be a hassle if you struggle to make ends meet. Under some circumstances, you may be able to have an overpayment waived, but it is not something to count on.
h3 id=”h-when-will-my-regular-monthly-benefits-begin”>When will my regular monthly benefits begin?
Regular monthly benefits usually begin the month after you receive your check for past due benefits, although some people actually get a check for regular monthly benefits first.
Such checks pay benefits for the previous month. For example, a first check sent in February will be for benefits you were owed in January.
h3 id=”h-will-i-be-eligible-for-medicare”>Will I be eligible for Medicare?
If you are under age 65 and receiving SSDI benefits, Medicare eligibility starts after you have received 24 months of Social Security disability benefits.
Medicare Part B, which pays for doctor visits, requires that you pay a premium. That premium will be deducted from your monthly SSDI check.
If you are disabled with low income and assets, other programs may be available to you to assist with paying medical expenses not covered by Medicare or pay the Medicare premium for you. To learn if you are eligible for such programs, contact your county welfare department.
If you already have health insurance, find out how Medicare works with your insurance policy. Health insurance policies are often written so that Medicare is the primary coverage. If so, your existing health insurance may only cover what Medicare does not pay for. Checking with your health insurance company is an important step when you get your Medicare card.
h3 id=”h-the-decision-cover-sheet-says-that-the-appeals-council-may-review-the-decision-on-its-own-motion-what-does-this-mean”>The decision cover sheet says that the Appeals Council may review the decision “On Its Own Motion.” What does this mean?
In rare cases, the Appeals Council may, on its own accord, review the Administrative Law Judge’s decision or dismissal within 60 days after the date of the ALJ finding.
The Appeals Council might review a random sample of SSDI decisions and dismissals that were not appealed. Other cases may be identified for review by the Appeals Council where a decision cannot be “effectuated”— carried out—due to clerical errors or other problems affecting the outcome of the case.
The Appeals Council will notify you of its decision to review your case by issuing a written notice of review by mail.
h3 id=”h-will-i-have-to-pay-taxes-on-the-social-security-disability-benefits-i-receive”>Will I have to pay taxes on the Social Security disability benefits I receive?
Typically a person does not have to pay taxes on Social Security benefits, but it depends on the amount of your total income.
- Couples filing a joint return will owe taxes if their combined income exceeds $32,000.
- Persons filing an individual tax return will owe taxes if their income exceeds $25,000.
- However, if a child receives benefits on a parent’s account, those benefits count only for establishing whether the child will be taxed on SSDI benefits received.
You may also owe taxes on Social Security disability benefits if you received a large check for past due benefits during the year. In this case, you still may not have to pay tax on your SSDI benefits.
The IRS has prepared a way to recalculate your back benefits and consider them received in the year you should have gotten them instead of in the current year. Contact the IRS for a copy of Publication 915.
If your Social Security disability benefits end up being taxable, you should note that a portion of the attorney’s fee may be deductible, but this depends on the 2 percent of adjusted gross income ceiling on miscellaneous itemized deductions.
If you have to repay a long term disability insurance carrier because you received Social Security disability benefits, you may get special tax relief. Ask the IRS for Publication 525.
SSA should send you a Form 1099 by February 1 of the year after your back benefits are paid. If you will have to pay taxes on your Social Security disability benefits, be sure to compare the information on the Form 1099 with the information on your Notice of Award. The Form 1099s from SSA can be incorrect. You will need to bring any errors to the attention of your tax preparer.
h3 id=”h-what-is-a-continuing-disability-review-cdr”>What is a “Continuing Disability Review (CDR)?”
SSA will periodically review your SSD or SSI case to determine whether you are still disabled. Most cases are reviewed at three years, but some cases are reviewed more often. Sometimes the decision will direct SSA to conduct a review at a certain time. The Notice of Award will tell you when to expect a review.
h3 id=”h-what-will-i-have-to-do-for-a-continuing-disability-review”>What will I have to do for a Continuing Disability Review?
You will be asked to complete a form about your medical treatment or work and how your condition has changed since you were found eligible for disability benefits.
h3 id=”h-what-if-the-ssa-finds-that-my-disability-has-ceased-but-i-m-still-not-able-to-work”>What if the SSA finds that my disability has ceased, but I’m still not able to work?
The notice that you will receive from SSA following a Continuing Disability Review will explain your appeal rights. Read this notice carefully. If you appeal within 10 days of the date you receive the notice, your benefits will continue during your appeal. Be sure to act quickly.
h3 id=”h-what-can-i-do-to-make-sure-my-disability-benefits-will-continue”>What can I do to make sure my disability benefits will continue?
The best thing you can do to make certain you keep getting disability benefits is to continue seeing your doctor.
Many who have chronic medical problems make the mistake of suspending or eventually discontinuing their doctor’s appointments and check-ups because no treatment seems to help. But this works against you: when SSA conducts its routine review of your case, there will be no medical evidence to support the fact that you are disabled.
Also important is for everyone – even healthy people – to have routine and thorough physical examinations after a certain age. This is even more important for people with chronic problems.
h3 id=”h-is-it-as-hard-to-keep-my-benefits-as-it-was-to-get-them-in-the-first-place”>Is it as hard to keep my benefits as it was to get them in the first place?
While many claimants faced extreme hardships during the years it took to apply and appeal, once found disabled, most claimants typically retain their benefits after winning a favorable decision.
h3 id=”h-what-can-i-do-to-make-working-with-ssa-easier”>What can I do to make working with SSA easier?
There may be problems at times. Here are some things you can try to lessen possible complications:
- Store all decisions, letters and notices you receive from SSA in a safe, secure place
- Read everything you get from SSA. The booklets that come with award letters and notices are well written and informative.
- When reading the booklets you receive, pay special attention to the kind of information you are required to report to SSA. Report that information promptly and in writing, and keep a copy with your Social Security papers.
Further reading:
Visit the Official Social Security website:
Official Social Security Website (Home Page)
Benefits for People with Disabilities (For Applicants & Claimants)
The Compilation of the Social Security Laws (The Social Security Act)
Reference Sources
- Social Security official website. Accessed January 1, 2016. https://www.ssa.gov/.
- Social Security Administration. Annual Statistical Report of the Social Security Disability Insurance Program, 2013. Accessed January 1, 2016. https://www.ssa.gov/policy/docs/statcomps/di_asr/2013/di_asr13.pdf
- United State Code of Federal Regulations. Accessed January 1, 2016. https://www.socialsecurity.gov/OP_Home/cfr20/cfrdoc.htm
- Marc Whitehead, The Social Security Disability Puzzle, 2010. Accessed January 1, 2016. /social-security-disability-ebook
- Marc Whitehead & Associates, Attorneys at Law, LLP. A National Disability Claims Law Firm. Accessed January 1, 2016. /
- National Organization of Social Security Claimants’ Representatives. Accessed January 1, 2016. https://www.nosscr.org/
- National board of Trial Advocacy. Accessed January 1, 2016. https://www.nbtalawyers.org/
- Bohr, Sarah H. and Harrington, Chantal J., Bohr’s Social Security Issues Annotated (Summer, 2000)
- Wilborn, Ralph, Wilborn’s, Social Security Disability Advocate’s Handbook, The Process of Unification Rulings, (1997, 1998)
- Bush, Thomas E., Social Security Disability Practice (2d ed. 2/92)
- Morton II, M.D., David A, Medical Issues In Social Security Disability (March 2004)
- O’Connor’s Federal Rules * Civil Trials (2010)
Table of Contents: Veterans Disability
Guide to Veterans Disability Compensation Claims
Chapter 2: Eligibility Requirements to Receive Veterans Benefits
- Meeting the “Military Service” Requirement
- Other Types of Military Service Can Make You Eligible for VA Compensation
- “Active Service” Requirements for Veterans Status
- How is “Active” Service Defined for Veterans Benefits?
- How the Character of a Discharge Affects a VA Claim
- How the Character of a Discharge is Determined for a VA Claim
Chapter 3: Veterans Compensation or Veterans Pension – Which to Apply For?
Chapter 4: Filing an Application for VA Compensation or Pension
Chapter 5: Types of Veterans Compensation Claims
- Is VA Compensation Only for Soldiers with Battlefield Injuries?
- What does “In The Line of Duty” mean?
- Requirements for Obtaining Service-Connected Disability Compensation
- Five Elements to Establish a Service Connected Claim
- Is the Veteran’s Disability Service-Connected?
- Proving Different Types of Compensation Claims
- Direct Service Connection
Chapter 6: Establishing Service Connection through a Medical “Nexus”
- Why Is Medical Evidence Needed to Prove a Nexus?
- How to Satisfy the Standard of Proof and the Evidence of Nexus
- Is there Ever a Time When Medical Evidence Is Not Required for Successful Veterans Claims?
- Presumptive Service Connection – Compensation for Presumptive Conditions
- What Is the Direct Service Connection?
- How to Prove the Direct Service Connection
- Chronicity
- Which Conditions Are Considered Chronic in a Veteran’s Disability Claim?
- Continuity of Symptomatology
- What Is Required to Prove Continuity of Symptomatology for VA Compensation Claims?
- Direct Service Connection for Diseases First Diagnosed after Service
- Which Conditions Diagnosed Post-Service Are Eligible for VA Compensation Claims?
- Five Ways to Establish the Service Connection
Chapter 7: The VA Assigns a Rating to Your Disability
- Schedule for Rating Disabilities
- The 10 Grades of Disability
Chapter 10: Presumptions and Rules in the VA Claims Process
Chapter 11: Appeal a Denied VA Claim
- The Process of Appeal
- Three Main Issues Examined in a VA Disability Decision
- If Your Claim is Denied: Notice of Disagreement (NOD) with the Regional Office
- How to File a Formal Appeal with the Board of Veterans Appeals (BVA)
- What Happens if the BVA Denies My Appeals Claim?
- When Should You Hire a VA Disability Attorney after a Denied Appeal?
- The Adjudication Process
- Duties of the VA in the Disability Claims Adjudication Process
- Adjudicating a Preexisting Condition
- When Is a Preexisting Condition Noted on Entry into Service Eligible for Compensation?
Chapter 12: How to Obtain Medical Evidence to Support Your Claim
- Other Strategies to Remember
- How to Prove Service Connection by Aggravation
- Case Law Regarding Aggravation
- Service Connection by Aggravation if Disability Was Not Noted During Entrance Exam
- Service Connection by Legal Presumption
- Requirements for VA Claims Using Service Connection by Legal Presumption
- Can the VA deny benefits in cases that use the service connection by legal presumption?
- Using Service Connection by Legal Presumption for Chronic Diseases
- Using the Service Connection by Legal Presumption for Tropical Diseases
- Service Connection by Legal Presumption for Former Prisoners of War
- Which Diseases Make Former Prisoners of War Eligible to Use the Service Connection by Legal Presumption?
- Service Connection by Legal Presumption for Radiogenic Diseases
- Amyotrophic Lateral Sclerosis (ALS) – Special Service Connection by Legal Presumption
- Other Instances of the Service Connection by Legal Presumption
- Victims of Agent Orange Exposure Are Entitled to Use the Service Connection by Legal Presumption
- VA Compensation Claims: What Is the Secondary Service Connection?
- How to Use the Secondary Service Connection to Argue VA Compensation Claims?
- Are Conditions Related to Tobacco Use Eligible for VA Claims?
- Getting Around the Tobacco Use Restriction
- Who Qualifies for Family Member Benefits?
- What Veterans Benefits Are Available to Qualifying Family Members of a Deceased Veteran?
- Death Benefits Based on a Service-Connected Condition
- How Do You Show That a Condition Is Eligible for VA Compensation Claims for Death Benefits?
- Death in Service – How It Affects a Family’s VA Claim for Death Benefits
- Special Survivors Veterans Benefits: The Restored Entitlement Program for Survivors (REPS)
- Which Surviving Spouses Are Eligible for REPS?
- Which Surviving Children Are Entitled to REPS?
- How Does Income Affect REPS Payments?
- Non-Service-Connected Veterans Benefits: What Is a Death Pension?
- What is the Improved Pension Program?
- The Surviving Child
- Are there Special Allowances for Family Members?
- How Can a Family Members Qualify for Special Allowance Veterans Benefits?
- VA Benefits for Children Born with Birth Defects in the Vietnam War Era
- Spina Bifida: What Requirements Must Be Met to Receive Increased Veterans Benefits?
- How To Claim Veterans Benefits for Children with Spina Bifida
- DIC Benefits for Surviving Family of Veterans Exposed to Agent Orange
- How Disability Claims for Agent Orange Cases Changed in the 90s
Chapter 14: Psychological & Cognitive Disabilities
- Disability Compensation for Mental Disabilities Other Than PTSD
- The 5 Ways to Service Connect a Mental Disorder in a VA Claim
- Glossary of Key Terms Used in Mental Disorder VA Claims
- Eight Categories of Mental Disorders Eligible for VA Compensation Claims
- Linking a Mental Disorder to Military Service
- Evaluate the Degree of Disability of a Mental Disorder
- Criteria Used to Determine Mental Disorders
- How a Soldier with Traumatic Brain Injuries Can Avoid a Veterans Claim Denial
- Evaluating Traumatic Brain Injuries Correctly to Avoid Claim Denial
- Who Is Eligible for PTSD Disability Claims?
- The Three Qualification Requirements for PTSD Disability Claims
- Special VA Compensation Claims Rules on Service Connection for PTSD
Chapter 15: Special Rules for Combat Veterans
- Why Do Combat Veterans Receive Special Treatment on VA Compensation Claims?
- What Do Combat Veterans Need to Prove to Get VA Compensation Claims Approved?
- How Do You Know If an Incident Occurred While “Engaged In Combat?”
- Ways to Corroborate a Veteran’s Statement about Their Combat Service
- Step by Step Application of How a Veteran’s Statement Is Analyzed
Chapter 16: Agent Orange Exposure
- Benefits Available to Veterans Exposed to Agent Orange
- Qualifying for VA Benefits after Herbicide Exposure
- Veterans Outside of Vietnam Eligible for VA Benefits Based on Herbicide Exposure
- Proving Exposure
- Proving You Are a Brown Water Naval Veteran
- New Diseases Added to VA Agent Orange Presumptive Illnesses List
- Recent Studies Regarding Possible Updates to Agent Orange-related Diseases
- Benefits for Surviving Family of Veterans Exposed to Agent Orange
- Effective Dates for Agent Orange Exposure in Vietnam
- Qualifying Diseases and Their Special Effective Dates for Agent Orange VA Compensation Claims
- Why Agent Orange Effective Date Rules for Death and Disability Claims Were Established
- The National Veterans Legal Services Program and AO Exposure Disability Claims
- What Communications Count as Disability Claims for Agent Orange-Related Diseases?
- Do Medical Records Count as Disability Claims?
- Other Requirements That Exist for Agent Orange VA Claims
- Category 1 Rules for Agent Orange VA Claims
- Effective Date Rule for Veterans Who Filed Category 1 VA Claims
- What If the Veteran Filed Multiple VA Claims that Fit within Category 1?
- Effective Date Rules for Category 2
- Do VA Claims for Service-Connected Burial Benefits Count as DIC Claims?
Chapter 17: Persian Gulf Veterans’ Claims
- How Presumptive Service Connection Affects Disability Claims
- How Section 1117 Affects Other Veterans’ Disability Claims
- Three Requirements for Establishing a Presumptive Connection When Making Disability Claims
- Are There Special Considerations for the Disability Claims of Certain Veterans?
- TBI Signs and Symptoms That Are Relevant to Veterans Disability Claims
- Environmental Hazards That Are Relevant to Veterans Disability Claims
Chapter 18: Upgrading a Veteran’s Discharge Status
- Can Upgrading a Discharge Make You Eligible for Veterans Benefits?
- Risks Associated With Upgrading a Discharge to Receive Veterans Benefits
- Is It Easier to Become Eligible for Veterans Benefits Through Discharge Upgrading or VA Adjudication?
- Choosing the Right Path to Be Eligible for Veterans Benefits
- Becoming Eligible for Veterans Benefits through Discharge Review
- What Factors Will Make a Discharge Review More Likely to Result in Veterans Benefits Eligibility?
Chapter 19: Get Help from an Accredited VA Attorney, Claims Agent or Representative
- Who Can Assist a Veteran with a VA Claim for Benefits?
- How Can I Find an Accredited VA Attorney, Agent or Representative?
- When Can the Accredited Attorney or Agent Charge Fees for Service?
- Secure Your VA Disability Benefits through an Accredited Veterans Claim Attorney, Agent or Representative
Guide to Veterans Disability Compensation Claims
Chapter 1: Introduction
Veterans within all branches of the U.S. armed forces return home dealing with disabling physical or psychological impairments. If you served our country in the military, you deserve to obtain the disability compensation you earned.
Whether you are filing your initial claim, or you are a family member seeking accurate information, this Guide to Veterans Disability Compensation will serve as a useful resource.
VA disability laws are complex. The claims process is frustrating to such a great degree that a veteran takes on a new battle, fighting the VA to win disability benefits. Many veterans end up getting denied on their first attempt.
Representation from an Accredited Attorney or Claims Agent is a veteran’s most critical aid in the successful preparation, presentation, and prosecution of a claim for benefits. The right assistance can ensure that you are following the claims process correctly, and that your case will be developed to have the best chance of getting your benefits approved in the shortest amount of time possible.
Find out more about getting accredited VA representation.
h3 id=”h-about-the-veterans-claims-process”>About the Veterans Claims Process
The U.S. Department of Veterans Affairs (VA) oversees veteran’s compensation. The central office in Washington, D.C. manages the activities of the VA Regional Offices (aka VARO or RO) and medical centers.
Two main duties of VA are to:
- provide veterans with medical and health care
- pay benefits to veterans.
The VA administers the following veterans’ benefits:
- Compensation for service-related disabilities,
- Pensions to eligible wartime veterans or their widows, and
- Compensation to spouses, dependents and survivors of veterans
h3 id=”h-the-vba-handles-claims-for-disability-compensation”>The VBA Handles Claims for Disability Compensation
Within the Central Office are the Veterans Benefits Administration (VBA) and the Veterans Health Administration (VHA). These two departments are responsible for providing these benefits.
The VBA handles monetary benefits including service connected disability compensation. To process a claim for veterans’ disability compensation, you will deal with the VBA.
h3 id=”h-the-va-s-definition-of-veteran-do-you-qualify”>The VA’s Definition of “Veteran” – Do You Qualify?
The first step in the claim process is to establish that you qualify as a veteran according to the VA’s definition. The VA defines a veteran as
“A person who served in the active military, naval or air services, and who was discharged or released under conditions other than dishonorable.”
The VA has the right to decide if your disability is a result of dishonorable service even if you have an honorable discharge.
h3 id=”h-the-4-steps-of-the-va-claims-process”>The 4 Steps of the VA Claims Process

- File a claim. Before the claims process can begin, your claim must be filed stating that you believe you are entitled to benefits based on a disability you are suffering. When you file a claim, don’t be too specific with medical terms. For example, if you claim you are suffering from spinal damage because you’ve been having a lot of back pain, but it is later determined that the damage is instead to your muscles, then it can lead to the denial of benefits by the VA.
- Develop a claim. After you file your claim, the VA is required to help you develop your claim. This means the VA will try to get your service medical records to follow up, as well as any other medical records that you mention. However, the VA will not look at your military records. If those are important to your claim, get them yourself. The VA will also give you a C&P Evaluation, or physical exam, for any current medical condition related to the claim, and provide a report with medical findings. The VA should also send you a letter explaining the VA claims process – how to back up and verify your claim, what the VA has done and will do, and what you need to do. Unfortunately, this “help” leaves a lot to be desired, which is why it is so important to find skillful representation.Note: an exception to the VA’s “duty to assist” veterans in their disability claims occurs with claims filed under the “Fully Developed Claims” Program.
- The Rating Decision. Once all the information is in, a Rating Decision will be made. For a favorable decision, you must have proven a service connection, percentage of disability, and an effective date of eligibility. Denial of veterans’ benefits will happen if any of these things are not met. However, each individual element can be appealed.
- Notice and Award Letter. Win or lose the claim, you will still get a letter from the VA notifying you. In fact, you need to make sure the VA has your current address or the VA simply won’t issue a ruling on your claim. Win and you’ll get an award letter that states your percentage of disability and tells you your effective date – the date from which you will start receiving benefits. The exact dollar amount of your compensation will be sent to you in a follow-up letter. If you receive a denial of veterans’ benefits, it’s in your best interest to get legal representation with the VA claims process. You have the right to appeal all rating decisions.
Chapter 2: Eligibility Requirements to Receive Veterans Benefits
In addition to meeting the VA’s definition of a veteran, you must meet the following criteria to confirm whether you will be classified as a veteran:
- You have served in any branch of the military,
- your military service was considered “active,” and
- Under what circumstances you were discharged
These three important points must be established if you are to begin the claims process. Dependents and survivors of veterans may also apply for benefits after establishing that their loved ones’ status met these three criteria.
If a veteran fails to meet the three basic eligibility requirements, he or she may still qualify for some benefits in certain cases.
Other factors might influence the types and amount of benefits that you, your spouse, or your dependents are eligible to receive. Examples include how long you actively served or if active service was during wartime.
h3 id=”h-meeting-the-military-service-requirement”>Meeting the “Military Service” Requirement
The VA will evaluate your experience to establish that your experience qualifies as military service. Serving in one of the five branches of the US Armed Forces is the most common form of military service. By serving with the US Army, Navy, Marine Corps, Air Force, or Coast Guard, you would generally meet the military service requirement.
Other ways of meeting the military service requirement is by serving in one of the five branches as a member of the Reserve, as a cadet or midshipman at a military academy, as a student in a prep school for one of the academies, or as a member of the Air or Army National Guard.
h3 id=”h-other-types-of-military-service-can-make-you-eligible-for-va-compensation”>Other Types of Military Service Can Make You Eligible for VA Compensation
There are some exceptions to the requirement of having served in one of the five branches of the US Armed Forces to be eligible for veterans’ benefits, as long as the VA has established that you meet the definition of a veteran.
Some examples of other services that might qualify:
- Commissioned full-time officers in the Public Health Service
- Commissioned full-time officers of the National Oceanic and Atmospheric Administration
- Commissioned full-time officers of the Environmental Science Services Administration
- World War II service in the Philippines’ organized military forces
- World War II service as an American Merchant Marine
- Pre-1943 service in the Women’s’ Army Auxiliary Corps
- Other service by civilians during a few specific periods of armed conflict
h3 id=”h-active-service-requirements-for-veterans-status”>“Active Service” Requirements for Veterans Status
Qualifying for what the VA regards as active service can be a more complicated process than meeting the requirement for military service.
For example, National Guard members are only eligible for veterans’ benefits during the period in which they are called into federal service.
h3 id=”h-how-is-active-service-defined-for-veterans-benefits”>How is “Active” Service Defined for Veterans Benefits?
Basically, “active” duty that qualifies a veteran to receive benefits is described as full-time service in any of the following:
- One of the five branches of the military
- As a commissioned officer for the Public Health Service or other federal service administrative organizations
- As a cadet or midshipman at a military academy
- In attendance at a military academy preparatory school, if the person had an active duty commitment
- During authorized travel to or from any of the above listed types of active service
Another circumstance of service is called active duty for training. This applies to members of the Reserve or National Guard, military prep school students, and some other veterans, which can qualify them as eligible for benefits. If the veteran was injured or killed during a training period, the veteran or surviving family may be able to receive benefits.
Another circumstance involves injury or death due to inactive duty for training. This can apply to National Guard members, Reservists, and some other veterans when benefits are considered. This category makes it possible for the VA to consider a veteran eligible for benefits if he or she becomes disabled or died in the line of duty as a result of health problems, such as stroke or heart attack, during training.
The VA will scrutinize the veteran’s service records to decide if his or her service fits the different categories of active service.
h3 id=”h-how-the-character-of-a-discharge-affects-a-va-claim”>How the Character of a Discharge Affects a VA Claim
The final requirement you must pass to meet the VA’s eligibility requirements to receive veterans’ benefits is: determining the character of your discharge.
For a veteran to be able to receive compensation, he or she must have been discharged “under conditions other than dishonorable.” While this might seem simple at first – the VA’s discharge categories do not conform exactly to the military’s discharge categories.
h3 id=”h-how-the-character-of-a-discharge-is-determined-for-a-va-claim”>How the Character of a Discharge is Determined for a VA Claim
The military’s discharge classifications are as follows:
- Honorable discharge (HD)
- Discharge under honorable conditions (UHC) or general discharge (GD)
- Discharge under other than honorable conditions (OTH) or undesirable discharge (UD)
- Bad conduct discharge (BCD)
- Dishonorable discharge (DD) or dismissal
The language used by the VA however, says that if a veteran is to be eligible for benefits, the discharge must be “other than dishonorable.” Veterans with the first three types of discharges (HD, UHC, or GD) almost always qualify for veteran’s benefits. People with dishonorable discharges almost never qualify.
It is possible to upgrade your discharge status before opening a case to determine benefit eligibility. Read more about Upgrading a Veteran’s Discharge Status.
h3 id=”h-the-insanity-exception-and-eligibility-for-benefits”>The Insanity Exception and Eligibility for Benefits
There may be exceptions to the rule that veterans can only claim VA benefits for disability if their discharges were “under conditions other than dishonorable.”
An example of this might be a case in which the veteran needing benefits is determined to have been insane at the time of his or her dishonorable discharge. VA compensation may be granted, when otherwise the character of the discharge would bar the veteran from receiving benefits.
h3 id=”h-claiming-veterans-benefits-using-the-insanity-exception”>Claiming Veterans Benefits Using the Insanity Exception
The first step to using the insanity exception in a veteran’s claim is having the medical evidence that the veteran was insane—as defined by the VA—during the time of the misconduct that led to his or her discharge.
It should suffice to prove that a mental disease-induced insanity was present at the time of the veteran’s misconduct, no matter if the misconduct was directly related to the insanity at the time it happened.
h3 id=”h-how-multiple-periods-of-service-impact-veterans-disability”>How Multiple Periods of Service Impact Veterans Disability
The process for establishing benefit eligibility for a veteran becomes even more complicated when a veteran has multiple periods of active service. For a veteran who has received different discharges for multiple service periods, this can become an issue.
If you were discharged for anything along the lines of mutiny, treason, or sedition, you clearly would not be eligible for benefits.
h3 id=”h-what-are-the-criteria-for-overlooking-a-disqualifying-discharge”>What Are the Criteria for Overlooking a Disqualifying Discharge?
VA considers certain criteria to overlook a disqualifying discharge. In most cases, if you are eligible to receive compensation benefits for a past period of service, you are generally able to keep those benefits—even if, during a later and separate period of service, you receive a dishonorable or disqualifying discharge. You are eligible for benefits for the service period ending under honorable conditions.
If you served back-to-back periods, these periods of enlistment may also be combined to cause a service commitment wherein you may be eligible for benefits.
For example, if the first period of service ended early and under honorable conditions, and the second period terminated under dishonorable conditions but enough satisfactory time had elapsed—when both periods of service are combined, the total satisfactory service is greater than or equal to the initial service commitment.
Chapter 3: Veterans Compensation or Veterans Pension – Which to Apply For?
Once you have made it past the initial “veteran” determination and have established eligibility, be sure you are applying for the appropriate veterans’ benefits. There is a difference between VA Compensation and VA Pension.
Visit the U.S. Department of Veterans Affairs website to get a better estimate of how much you can expect if your claim is approved. Online rate tables for compensation and pension are provided. Widows and children of disabled veterans may qualify for compensation and pensions as well.
h3 id=”h-the-difference-between-compensation-and-pension”>The Difference between Compensation and Pension
Compensation is a monthly benefit paid to a veteran as a result of a “service-connected” injury, disease or condition. For a condition to be judged “service connected,” it must be sustained or aggravated as a result of service to the military.
Compensation is not based on need, nor is it restricted to any particular period of service. All of the evidence on record will be examined to evaluate whether a veteran’s disabling condition should be regarded as service connected.
Pension is needs-based welfare. Pensions are paid when any total disability – whether it is service-connected or not – causes the veteran to require financial assistance.
h3 id=”h-a-closer-look-at-compensation”>A Closer Look at Compensation
Veterans’ disability compensation can be between 10 percent and 100 percent, depending upon the percentage of disability. You may be given a 100 percent rating even if you have less than 100 percent disability if you are unable to work due to the service-connected disability.
Veterans who are considered extremely disabled may qualify for more than 100 percent.
Retired veterans who are found disabled have been subjected to offsets in their retired pay regarding compensation, but this is slowly being phased out.
To receive service connected disability compensation a veteran must show:
- The veteran’s discharge was other than dishonorable;
- The disease or injury was incurred or aggravated in the “line of duty;” and
- The disability was not a result of willful misconduct or drug/alcohol abuse.
Help Tips:
- Severe disabilities may get Special Monthly Compensation (SMC)
- Veterans who receive a 30% or more rating are entitled to additional family compensation
- If a veteran’s death is service connected, the family may receive Dependency and Indemnity Compensation (DIC).
- A military finding of “incurred in line of duty” can be binding on the Department of Veterans Affairs
- In the Line of Duty means:
- The injury or disease was incurred or aggravated during a period of active service, unless a result of willful misconduct or drug/alcohol abuse;
- Encompasses anything that happened while in service. There is no stipulation that the veteran had been performing military duties. Injury could have occurred while the veteran was off duty and off base.
- Includes latent medical conditions that were not discovered until much later.
Read about the Types of Veterans Compensation
h3 id=”h-a-closer-look-at-pension”>A Closer Look at Pension
VA Pension is only available to certain veterans, such as those who served during a period of war and are totally disabled from any type of work. The disability does not need to be service connected.
Pension payments are considerably less than VA Compensation payments. Pensions are paid in a flat amount that is offset by other income dollar-for-dollar. Nevertheless, some favorable presumptions exist under the pension program.
Read more about Veterans Pension Program.
Chapter 4: Filing an Application for VA Compensation or Pension
Begin the claims process by applying in one of the following ways:
h3 id=”h-file-for-veterans-compensation”>File for Veterans Compensation
- Submit a Paper Application:
For Veterans Application for Compensation use the paper VA Form 21-526EZ. Download copies at the U.S. Department of Veterans Affairs website, or visit your closest VA Regional Office. - Apply Online at wwww.eBenefits.va.gov.
The eBenefits website is a service of the Department of Veterans Affairs and the Department of Defense.
h3 id=”h-file-for-veterans-pension”>File for Veterans Pension
- Submit a Paper Application:
For Veterans Application for Pension use VA Form 21-527EZ. Download copies at the U.S. Department of Veterans Affairs website, or visit your local VA Regional Office. - Apply Online at https://vabenefits.vba.va.gov/vonapp/default.asp
Use the Veterans On-Line Application (VONAPP) Website for Pension claims. (You do not use VONAPP to submit a Compensation claim.)
h3 id=”h-file-using-accredited-representation”>File Using Accredited Representation
- Appoint a VA-accredited attorney or agent to act on your behalf in the preparation, presentation, and prosecution of claims for VA benefits. Veterans seeking representation may rely on information found on the VA’s website here: Office of General Counsel (OGC) Search for Accredited Attorneys, Claims Agents, or Veterans Service Organizations (VSO) Representatives.
File Using the “Fully Developed Claim” (FDC) Program for Fast-Track Decisions
Recently introduced to the disability claims process is the concept of the “Fully Developed Claims” (FDC). Fully Developed Claims are part of the VA’s response to expediting disability compensation claims and dealing with the tremendous backlog. Claims submitted under the FDC program may be processed by the VA within 30-60 days of submission.
Successful original claims under the FDC program will result in an extra year’s worth of compensation. Once you begin your FDC, you have one year to complete it online. If VA approves your claim, you will be paid back to the day you began your claim.
As a disabled veteran filing a FDC, you must assume the burden of collecting the necessary documentation, and assembling and preparing your claim without any help from the VA. You waive your rights to VA’s normal “Duty to Assist” you in your claim.
The theory is that because your claim is fully developed – it is comprehensive and perfected – you are providing everything the VA needs to make a just decision. Aside from ordering medical exams and possible Federal records, all the VA has to do is review your claim and make a determination on it.
While this method does not guarantee an award of benefits, VA hopes the fast track, and for original claims additional benefits, are sufficient incentives for veterans to navigate the military records system and undertake the Veterans claims process on their own.
In theory, because the veteran does all the heavy lifting without VA’s assistance, the veteran reaches a fast and accurate decision. In reality, a disabled veteran may or may not have the ability or fortitude needed to understand, locate and assemble all necessary evidence on their own to truly develop a winning claim.
If the VA decides your claim is not fully developed (is lacking necessary evidence) the VA would take your claim out of the FDC program and the claim would then undergo the regular claims process.
Fully Developed Claims are optional, and may be filed for
- veterans disability compensation
- survivor benefits
- veterans pension
To file an FDC, VA advises to file electronically at eBenefits.gov. If you file a paper FDC for VA disability compensation, you will need to complete VA Form 21-526EZ and visit your local RO.
CAUTION: Submit your application in one way only; do not submit both online and by mail or in person. This can cause confusion about your claim and will slow down the process even more. Keep a copy of each form, document and record that you submit to the VA. This is critical in the event your claim is denied; plus the VA has been known to lose information.
Make sure the claim is complete: submit all relevant information.
Attach copies of all medical evidence that supports your claim. This includes copies of military service records, discharge papers, doctor and hospital records, diagnostic reports, and medical evidence of a link or “nexus.”
Also provide all dependency records, such as a marriage certificate or children’s birth certificates. Take extra care to follow all instructions and answer questions accurately and completely in order to speed the process.
When you have all the necessary VA documents and have completed the application, you can submit it by
- Mail or take the application to the closest VA Regional Office.
- Submit the Online Application
- Fax the documents. To get a fax number for the VA Regional Office that is handling your claim, contact the National Call Center at 1-800-827-1000.
- Work with an Accredited Representative – Your VA-accredited attorney or agent will assist in all matters on your behalf in claims for VA benefits.
REMEMBER! Do not submit both a mail and online application. Doing so could cause confusion about the claim. And remember: always keep a copy of all completed forms and materials that you provide to the VA for your records. This can be beneficial in case you are denied disability benefits or if the documents are lost.
h3 id=”h-required-medical-examination”>Required Medical Examination
When you begin the VA claims process, you will be subject to an examination at a VA medical center. The examination is offered for free to all veterans who are concerned that their ailments are related to their military service.
During the examination, an approved examiner conducts a physical review of your symptoms and takes note of all your complaints. Once the examination is complete, the results are considered among the other evidence you provide with your disability claim.
h3 id=”h-developing-your-claim-to-prove-eligibility-for-va-disability”>Developing Your Claim to Prove Eligibility for VA Disability
The standard of proof for a VA disability claim says the VA must give the disabled veteran the benefit of the doubt if the evidence on both sides is equal. Even so, the burden is still on the veteran to make a credible, convincing case.
The VA’s evaluation is mostly based on service records, but it is the disabled veteran who must assemble and submit those documents. The first step is to submit military records that prove the location and length of your active duty service, as well as the type of discharge you received.
Do this in one of three ways:
- Submit the original document from your service department
- Submit a certified copy of the original document
- Authorize an accredited agent to submit a certified copy
If for some reason your records do not reach the VA, the Board is obligated to ask for the relevant documents directly from your service department.
If your service document does not accurately reflect your service, you may submit what is referred to as “lay evidence.” This includes medical records and personal statements, to help make your case. Veterans’ claims are often won or lost based on the lay evidence submitted.
If at any time you are uncertain about what is required to produce an accurate, winning claim, consult an accredited VA attorney or agent.
h3 id=”h-talk-with-someone-at-the-va-about-the-claims-process”>Talk with Someone at the VA about the Claims Process
There are 22 forms a typical disabled veteran must fill out. Your paperwork goes through 8 levels of command and 16 different information systems.
You can always contact the VA on the VA website, https://www.benefits.va.gov/benefits/, by visiting the closest VA Regional Office or by telephone at 1-800-827-1000 if you have any questions or concerns about your claim.
Chapter 5: Types of Veterans Compensation Claims
The following describe the various forms of compensation available to veterans, and their eligibility requirements.
h3 id=”h-is-va-compensation-only-for-soldiers-with-battlefield-injuries”>Is VA Compensation Only for Soldiers with Battlefield Injuries?
Regulations that govern VA compensation state that, for service connected disability benefits, the medical condition a veteran has sustained must have been “suffered or contracted in the line of duty.” This includes any preexisting conditions that were made worse in the line of duty.
h3 id=”h-what-does-in-the-line-of-duty-mean”>What does “in the line of duty” mean?
A disability that is service connected means a death or disability was incurred or aggravated during active service “in the line of duty.” In the Line of Duty means:
- The injury or disease was incurred or aggravated during a period of active service, unless the injury or disease a result of willful misconduct or drug/alcohol abuse;
- Anything that happened while in service. There is no requirement that the veteran had performed military duties. Injury could have occurred while you were off duty and off base.
- Latent medical conditions that were not detected until years later. For example, a Veteran that sustained head trauma in bike accident while on leave – but did not experience problems until years later could qualify as having a service connected injury.
h3 id=”h-requirements-for-obtaining-service-connected-disability-compensation”>Requirements for Obtaining Service-Connected Disability Compensation
You must comply with three central requirements in order to qualify for service-connected disability compensation. The veteran must show:
- competent evidence of a current disability;
- medical evidence of an in-service occurrence or aggravation of the disease or injury. In some cases, lay evidence may also be accepted;
- proof that there is a link between the in-service injury and the current disability by providing competent evidence.
The following explains these fundamental requirements:
- Current Diagnosis. Many benefits are denied because the veteran wrongly believes that he or she is entitled to compensation just for being injured while were serving in the armed forces. This is incorrect. For VA compensation claims to be granted, the veteran must currently suffer from a medically diagnosed injury. Even if you were severely injured, if the doctors assess that your injury is healed, you will not qualify for benefits.
- In-Service Event. For the VA to award compensation, you also need to prove that some event during your service (such as a disease or an injury) caused the current disability. There must be medical evidence of an in-service occurrence or aggravation of the disease or injury.The VA will scrutinize your service medical record for evidence, and investigate your case to assess whether any conditions diagnosed during your service did not pre-exist your military service. If you cannot prove that your service aggravated the condition, benefits may be denied. It may be possible to submit lay evidence to support your claim, and the VA may allow “proof” in the form of private medical records or witness statements.
- A Nexus (Link) between Current Diagnosis & In-service Event. The veteran must provide competent evidence showing a link between the in-service injury and the current disability. In other words, VA compensation claims not only need to show that the original injury occurred during your service (or that a previous injury was aggravated), they also must provide medical evidence showing that your current disability stems from that original incident.This is proved by what is known as “continuity of symptomology.” Basically, you need to show that the original incident caused a particular condition for which you received treatment, and then you must show how that treatment has continued. If you stop receiving treatment for a time, or if more than a year passes between the time you are discharged from service and you file your claim, proving the existence of a “nexus” becomes harder. Many denied veterans benefits are often the result of an inability to prove that the nexus exists.
Remember that the only evidence considered acceptable in deciding most claims is medical documentation. Obtaining clear and thorough evidence from a doctor or other medical professional is critical to winning VA disability compensation.
h3 id=”h-five-elements-to-establish-a-service-connected-claim”>Five Elements to Establish a Service Connected Claim
There are “five elements” to establish a service-connected claim for a veteran’s disability benefits:
- Veterans status
- The existence of a current disability
- A connection between the veteran’s service and the current disability
- The degree of disability
- The effective date of the disability
The VA is required to assist you in obtaining the evidence you need to win your disability claim. But remember: ultimately it is your responsibility to provide the evidence that meets the burden of proof to successfully qualify for compensation payments.
Exceptions to the VA’s “duty to assist” rule are claims filed under the Fully Developed Claims (FDC) process.
h3 id=”h-is-the-veteran-s-disability-service-connected”>Is the Veteran’s Disability Service-Connected?
The Code of Federal Regulations (CFR) outlines basic guidelines for disability-related veterans benefits. These guidelines are used to evaluate whether the injuries or diseases that are shown on the veteran’s service records should be considered service connected.
Each disabling condition for which a veteran is seeking compensation must be considered based on the following criteria:
- The places, types, and circumstances of the veteran’s services
- The official history of each organization the veteran has served in
- The veteran’s full medical records
- Any and all lay evidence that is pertinent to the veteran’s disability claims
h3 id=”h-proving-different-types-of-compensation-claims”>Proving Different Types of Compensation Claims
While the Direct Service Connection claim may be the type most veterans are familiar with, there are various other types of VA compensation claims. The way you prove that you deserve benefits in each case is not the same.
The different VA compensation claim types are:
- Direct Service Connection
- Secondary Service Connection
- Claims for Increased Disability Ratings
- Reopened Claims
- 1151 Claims
- Dependency and Indemnity Compensation (DIC) and Accrued Benefits
- Clear & Unmistakable Error (CUE) Claims
- Non-Service-Connected Pension Benefits
Below is a description of each type of compensation claim in detail.
h3 id=”h-direct-service-connection”>Direct Service Connection
While you may file a direct service connection claim at any time, the longer you are out of the service before filing the claim, the harder the case becomes to prove. The three requirements to prove to show you deserve VA benefits are: current condition, precipitating event that occurred during service, and “nexus.”
The direct service connection is also the first strategy that VA board members are trained to use when evaluating claims. You must do everything possible to establish that the link between your disability and a presumptive service incident qualifies as a direct service connection.
Important Requirements of Obtaining Service Connection Compensation
- Veterans Status (not dishonorably discharged)
- Medical Diagnosis of Current Disability.In the original claim (not a reopened claim), the VA is required to help you obtain a Medical Diagnosis
- Medical Evidence (and sometimes lay evidence) of an in service occurrence/aggravation of disease or injury.
- Note that if you are a combat veteran, then VA must accept your statement of occurrence in combat as true.
- Medical evidence of a link or “nexus” between an in service occurrence and current disability
- If a nexus is established, then the VA must establish a Rating Percent
- If a nexus and a rating is established, then the VA must assign an effective date (the date retroactive benefits will begin).
- The Standard of Proof is “as likely as not” as to each issue. This tie goes to the vet.
- There is no requirement that the VA take your treating physician’s opinions as true (unlike the Social Security Disability system).
Disabilities that Are Not Service Connected
- Congenital (birth) defects
- Refractive eye errors
- Some personality disorders and mental deficiencies
h3 id=”h-secondary-service-connection”>Secondary Service Connection
When a veteran has a condition directly connected to his or her service and later suffers from a different medical condition that developed because of the original condition, it is possible to get veterans benefits for both the primary and secondary disability. For example, if you developed diabetes through chemical exposure during service and then develop heart disease later in life as the result of the diabetes, the secondary service connection might apply.
In order for a secondary condition to qualify for veterans benefits, a vet must 1) already have a condition deemed to be service connected, 2) currently be suffering from a second condition, and 3) obtain a doctor’s opinion stating that the secondary condition “as likely as not” developed as a result of the original, service-connected disability.
It is very important to be aware of and actively pursue benefits for secondary conditions because they can often be more costly and damaging than the original issue.
h3 id=”h-claims-for-increased-disability-ratings”>Claims for Increased Disability Ratings
It is common for a veteran’s level of disability to increase over time. If you believe the level to which you are disabled has increased since you were first given a “percentage of disability” that was calculated by medical definitions, you may return to the VA and ask for your compensation to be increased. This will require the VA to examine you and give you a diagnosis.
There is no real downside to requesting increased compensation for a worsening condition. It may also serve as an opportunity for the VA to notice secondary conditions.
Learn more about Increased Disability Ratings.
h3 id=”h-reopened-claims”>Reopened Claims
If your claim for veterans’ benefits was denied originally, and was not granted on appeal, you may be able to reopen the claim.at a later time even after the appeal period has expired. You may also reopen a claim if you missed the appeal deadlines. In order to reopen your claim, you first need to show new, highly relevant evidence that was not considered during the original claim. This new evidence should directly relate to the reason the initial claim was denied.
h3 id=”h-1151-claims”>1151 Claims
An 1151 claim may be filed if a veteran is injured as a result of treatment received at a VA Vocational Rehab program or in a VA medical facility. There is no statute of limitations for filing an 1151 claim.
In addition to the 1151 claim, a malpractice claim may be entered under the Federal Tort Claims Act. As a civil lawsuit, this type of claim will be held to the relevant statute of limitations, so the claim must be filed in a timely manner. Any money received from a malpractice claim would be deducted from the 1151 claim.
h3 id=”h-dependency-and-indemnity-compensation-dic-and-accrued-benefits”>Dependency and Indemnity Compensation (DIC) and Accrued Benefits
A spouse, dependent child or parent of any deceased veteran who qualified to receive service connected compensation may be awarded Dependency and Indemnity Compensation. To qualify,
- the veteran’s death must have been due to his or her service-connected disability – OR –
- the condition had to have been 100% disabling for 10 years prior to the veteran’s death.
Normal service-connected claims often become DIC claims because many veterans die while waiting to receive the benefits to which they are entitled.
h3 id=”h-clear-unmistakable-error-cue-claims”>Clear & Unmistakable Error (CUE) Claims
Clear and Unmistakable Error (CUE) claims happen when veterans believe they were denied disability benefits due to VA mistakes on their original claim. Winning this claim is a significant victory because if you do, you will start getting monthly benefits and receive back pay (sometimes from several years!) from the date the original claim was filed.
You can imagine that CUE claims are quite difficult to prove. You must show that either the adjudicator did not have the correct facts to decide the case (not based on new evidence, but on what was known then), or that the VA’s provisions were not followed, and that resulted in changing the outcome of the case. Only one CUE claim is allowed per condition, so it’s not something you want to go into lightly. These types of claims can be made at any time.
h3 id=”h-non-service-connected-pension-benefits”>Non-Service-Connected Pension Benefits
Technically this is a claim for pension. Many veterans’ claims of this sort are denied due to neglecting to show one of the following three elements: 1) that your current disability totally prevents you from working, 2) that the allowed maximum income for pensions is higher than what you receive, 3) and that you served during wartime.
Chapter 6: Establishing Service Connection through a Medical “Nexus”
Making successful VA compensation claims is dependent on several factors. Perhaps the most important of these is establishing a service connection, or a “nexus,” between your current disability and a triggering incident during your period of military service.
The main cause of denied VA claims is a lack of medical evidence used to provide proof of this nexus.
h3 id=”h-why-is-medical-evidence-needed-to-prove-a-nexus”>Why Is Medical Evidence Needed to Prove a Nexus?
Veterans are often called to testify during hearings for VA compensation claims about their symptoms and the service-connected incidents that led to their symptoms. Some of your testimony may be deemed “competent evidence” if you appear capable of identifying the medical condition in question. However, most cases involve conditions in which a medical expert must provide specialized expertise for a diagnosis. In these instances, the fact that you may not be a medical expert makes your testimony invalid when it comes to proving the service connection.
Again, a veteran’s testimony or “lay evidence” (evidence provided by someone without medical expertise) can only be used to establish a diagnosis. It does not identify the connection between diagnosis and an inciting service-connected incident. Most VA compensation claims are lost due to lack of sufficient medical documentation of the nexus. An accredited VA attorney or agent will be aware of this requirement and can help you provide the proper medical evidence of the service connection.
h3 id=”h-how-to-satisfy-the-standard-of-proof-and-the-evidence-of-nexus”>How to Satisfy the Standard of Proof and the Evidence of Nexus
In reference to the standard of proof, VA regulations state that if the evidence regarding any part of your claim is equally balanced between favorable and unfavorable proof, the VA must give you, the claimant, benefit of doubt and rule in your favor. Thus, any “reasonable doubt” created because of an equal lack of proof on both sides of the argument means that the veteran wins the case.
The same rule applies specifically to the nexus of proof requirement. To win your case and start receiving veterans benefits, the medical opinion you provide to prove the nexus need only state that it is “as likely as not” that your current disability and the precipitating service incident are connected. This removes the burden of providing absolutely definitive proof from medical experts and makes it much easier for veterans to make successful VA claims. A 50-percent chance of connectivity is all that’s required.
An ideal situation would of course be to develop a strong case with enough proof on your side of the argument that the reasonable doubt rule would not need to be invoked.
h3 id=”h-is-there-ever-a-time-when-medical-evidence-is-not-required-for-successful-veterans-claims”>Is there Ever a Time When Medical Evidence Is Not Required for Successful Veterans Claims?
Yes—a few situations exist where medical opinion states the link between the disability and precipitating service incident is not required.
If your current disabling condition is clearly the result of an injury that took place during service (such as an amputation after an in-service event), you are not required to provide a medical opinion proving the nexus. Lay evidence is generally sufficient in such cases for the VA to make a determination of an award. As long as the disability in question is readily identifiable to someone without medical training, lay evidence will be all that is required for the VA’s favorable ruling.
Another situation in which medical evidence may not be required is when the disability currently suffered by the veteran is chronic and was previously diagnosed during military service. In cases like this in which you have already left the service, you need to provide a diagnosis of the same chronic disease identified during active duty. It is possible that a diagnosis without any additional medical opinion or analysis will be enough for the VA to make a favorable ruling.
Read more about chronic conditions and chronicity.
h3 id=”h-presumptive-service-connection-compensation-for-presumptive-conditions”>Presumptive Service Connection – Compensation for Presumptive Conditions
Another circumstance during which a nexus of evidence may not be required to receive veterans’ benefits occurs when the veteran’s disability qualifies for the presumptive service connection.
The VA presumes that certain circumstances of a veteran’s military service caused specific disabling conditions. The VA provides a list of disabilities that automatically qualify for veterans benefits as long as the condition in question was diagnosed during the specified presumptive period.
As an example, veterans who served in the Persian Gulf War or Operations Iraqi Freedom or Enduring Freedom would not need to provide evidence of linkage for chronic fatigue syndrome or fibromyalgia diagnosed during their service in Southwest Asia since it is on the VA’s approved list.
Even though the VA defers the nexus of evidence requirement in these cases, it is in your best interest to be ready to provide detailed medical opinions in the case that the VA does not make the assumed allowance.
h3 id=”h-what-is-the-direct-service-connection”>What Is the Direct Service Connection?
The phrase “direct service connection” means the veteran’s current disability is a direct result of an incident that occurred or a disease that was diagnosed during the period of military service.
This is the first method to which most veterans turn when establishing a link between a service incident and disability. It is also the first strategy that VA board members are trained to use when evaluating claims. It is imperative to establish that the link between your disability and a presumptive service incident qualifies as a direct service connection.
h3 id=”h-how-to-prove-the-direct-service-connection”>How to Prove the Direct Service Connection
You normally need have three items of evidence to support service connection:
- Medical documentation of the current disability
- Lay or medical evidence of having suffered an injury, sickness or event while actively serving,
- An expert medical opinion linking the disability to the injury, sickness or event.
Successful VA compensation claims need to meet all three of these condition.
Two special provisions exist under which a direct service connection can be established without the presence of item (2) evidence of in-service incident or injury (3) medical assessment linking injury to disability. These situations occur when the veteran can prove “chronicity” or “continuity of symptomatology” and are explained below.
h3 id=”h-chronicity”>Chronicity
“Chronicity” is a policy through which you can argue for VA compensation without providing medical evidence of a nexus.
Chronicity applies when the veteran is eligible to receive benefits because his or her disability is a chronic (long-lasting) condition that was diagnosed during a period of service or a designated presumptive period. Chronicity can make it more straightforward for veterans with long-term conditions to successfully argue their disability claims and receive the veterans’ benefits they deserve.
In the event your disability might be considered chronic by the VA, you’ll need to provide medical evidence showing that you were diagnosed with the condition during service and that a recent medical examination found that you continue to suffer from the same condition.
The direct service connection is presumed under the theory of chronicity. You would still provide statements from medical professionals, but you are not required to present records other than your diagnoses. You will not need the detailed medical opinions and analysis required for other veterans compensation claims.
h3 id=”h-which-conditions-are-considered-chronic-in-a-veteran-s-disability-claim”>Which Conditions Are Considered Chronic in a Veteran’s Disability Claim?
The VA’s list of chronic conditions consists of numerous impairments, including particular forms of cancer, Parkinson’s disease, tuberculosis, epilepsy, and many other ailments. Consider consulting a qualified disability lawyer who can help you determine whether the VA recognizes your condition as chronic.
There are two ways to establish that your current disability meets VA’s theory of chronicity.
- There are two ways to establish that your current disability meets VA’s theory of chronicity. Demonstrate that your disease or condition is on the list of conditions recognized by the VA as chronic. The period of time that has passed between your time of service and the time you apply for VA compensation does not matter. If a veteran’s condition is on the list, he or she can prevail in a claim for disability benefits, as long as the veteran can successfully demonstrate diagnoses of the same chronic condition during service and currently.
- A veteran may be able to successfully argue his or her case and receive veterans’ benefits if the veteran has a chronic condition that is not on the VA’s approved list.
In both cases it is wise to seek help from a qualified veterans’ advocate or lawyer—either to ensure your condition fits the requirements, or if the impairment is not on VA’s list of chronic impairments, to develop evidence based on medical reference material or doctors’ statements.
h3 id=”h-continuity-of-symptomatology”>Continuity of Symptomatology
The “continuity of symptomatology” is another policy that may be used to argue VA compensation claims without providing medical evidence of a nexus. This applies to circumstances in which a chronic condition probably manifested during service but was not specifically diagnosed during that time.
The key to proving that continuity of symptomatology applies to your case lies in the description of your symptoms. Although your current disability need not have been diagnosed during your period of military service, you will be required to show evidence that the symptoms similar to your current ones were present and “noted” during service.
The U.S. Court of Appeals has ruled that favorable claims using continuity of symptomatology and the direct service connection do not require additional proof of a nexus of evidence. Even the court’s ruling is a little misleading, though.
Most cases actually do require a medical opinion linking the current disability with the symptoms present during service except in a few rare cases where lay evidence is enough to prove that the condition exists.
h3 id=”h-what-is-required-to-prove-continuity-of-symptomatology-for-va-compensation-claims”>What Is Required to Prove Continuity of Symptomatology for VA Compensation Claims?
To successfully show continuity of symptomatology, three types of evidence are needed:
- Proof that the symptoms of the current disability were “noted” during the period of service
- Proof that these same symptoms continued after the period of service ended
- Medical documentation (or in some rare cases, lay evidence) that a link exists between the post-service symptoms and the current disability
Do not rely on the evidence of continuous symptoms alone as proof. The third element of evidence, establishing a link by a medical authority, is required to successfully argue a veteran’s compensation claims using continuity of symptomatology.
h3 id=”h-direct-service-connection-for-diseases-first-diagnosed-after-service”>Direct Service Connection for Diseases First Diagnosed after Service
If you discover that your disabilities that are diagnosed after serving were caused by service incidents, the VA holds that the direct service connection can be granted when you prove your condition first began during military service—regardless of how much time has passed since your military service period ended.
To establish a direct service connection in this case, the veteran needs to prove that a nexus of evidence exists connecting the current disability to an incident or illness that occurred during time of service.
If a medical expert finds that the current disability presented within a certain amount of time after your period of service—depending upon the type of medical condition—a presumptive service connection may exist.
If so, service connection will be automatic and will not require nexus of evidence. A qualified VA representative will be able to advise whether your condition qualifies for the presumptive service connection.
h3 id=”h-which-conditions-diagnosed-post-service-are-eligible-for-va-compensation-claims”>Which Conditions Diagnosed Post-Service Are Eligible for VA Compensation Claims?
Any impairment that is proven to be linked to a veteran’s period of service can be eligible for a direct service connection, no matter when the disease manifests during the veteran’s lifetime. Winning these types of VA claims requires gathering a large amount of medical documentation.
Some of the most common conditions eligible for the direct service connection are:
- Cancers caused by exposure to harmful substances
- Mental disorders, such as posttraumatic stress disorder or panic attacks
- Degenerative diseases or other conditions caused by serious injuries
- Hearing loss from prolonged exposure to loud noises
h3 id=”h-five-ways-to-establish-the-service-connection”>Five Ways to Establish the Service Connection
To recap, a veteran has five strategies to prove the link between military service and a current disability:
- Direct service connection: a clear, causal link between a veteran’s current impairment and an event that occurred during the period of service
- Aggravation: a condition that was present before the veteran’s period of service but was worsened during duty, resulting in the present disability
- Presumptive service connection: although the condition cannot be directly linked to an incident during service, VA regulations state a presumed connection based on the type of disability and date of service
- Secondary service connection: the veteran’s current impairment is not directly connected to a service incident but is a direct result of a medical condition that is clearly linked to the veteran’s period of service
- An 1151: The current disability resulted from an injury sustained as a result of VA healthcare, a VA rehab or training facility, or a VA sponsored work therapy program. (This strategy does not require a service connection and is a unique circumstance made valid for compensation by an act of Congress).
Chapter 7: The VA Assigns a Rating to Your Disability
With service connection confirmed, the VA will assess the amount of monthly compensation payment you are entitled to. The benefit amount is based on the extent your disability would hinder the average person earning an income sufficient to live on in the United States.
The individual earning ability of each veteran is not part of this consideration. So a claim for compensation for a physician is calculated the same way as it is for a clerk.
h3 id=”h-schedule-for-rating-disabilities”>Schedule for Rating Disabilities
To grant your claim and award a benefit, VA “rates” your disability.
The VA Schedule for Rating Disabilities is VA’s guide for evaluating the severity of mental and physical disabilities resulting from all manner of injuries or diseases that occurred as a result of military service.
In the Schedule, impairments are categorized based on the part of the body, or body system, impacted. Examples are musculoskeletal, respiratory, digestive, infectious diseases, etc.
Each category lists groups of medical issues. Each group of medical issues lists the possible diagnoses. Each diagnosis has a diagnostic code that defines the symptoms that are required for different ratings of disability.
View the current schedule at the Electronic Code of Federal Regulations Title 38, Chapter 1 Part 4, Schedule for Rating Disabilities.
h3 id=”h-the-10-grades-of-disability”>The 10 Grades of Disability
The level of severity of your disability is expressed as a percentage rating – which regulates the amount of compensation.
The VA applies 10 graduating levels of disability expressed in increments of 10 percent: 0%, 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, 90%, and 100%. The higher the disability evaluation grade, the higher the veteran’s monthly payment.
A grade of 100% means the veteran is totally disabled and unable to work, and the veteran is entitled to the highest possible monthly compensation. Veterans with a 0% disability grade may still be entitled to significant benefits including VA health care, job retention rights, and priority when applying for state or federal jobs.
h3 id=”h-claims-for-increased-disability-ratings-1″>Claims for Increased Disability Ratings
If your service-connected condition worsens, you may apply for an increase in grade. In this case, you would go back to the VA and request an increase in your compensation. The VA will examine you and give you a diagnosis.
A favorable re-evaluation can mean a significant increase in compensation; it also offers the VA an opening to observe secondary conditions.
Seven Points to Remember about the VA Schedule for Rating Disabilities:
- A grant of compensation usually results in monthly payments
- Payments are designed to offset the degree of disability for the average worker
- VA does not consider the individual veteran’s earning capacity
- All veterans are paid the same for the same rating, regardless of the condition
- VA adopts a “Schedule of Ratings in reduced earnings capacity for specific injuries”
- Ratings are from 0 percent to 100 percent in 10 percent intervals
- A 0-percent rating gives no monthly compensation, but can provide other benefits such as preference in federal/state employment, job retention rights, and VA health care
h3 id=”h-not-satisfied-with-your-disability-rating”>Not Satisfied with Your Disability Rating?
You may find yourself with a lower disability rating than you believe your situation deserves. Get information about what to do if you disagree with your VA disability rating.
Chapter 8: Effective Dates
The VA has rules for establishing effective dates that cover all types of claims, including original claims, reopened claims, and claims to increase disability ratings.
h3 id=”h-effective-date-rule-for-original-va-claims”>Effective Date Rule for Original VA Claims
The general rule for determining the effective date for an original claim is: the VA looks at the date it received the claim and the date that the entitlement to the benefit “arose.” The later of these two dates is the effective date.
h3 id=”h-effective-date-for-reopened-va-claims”>Effective Date for Reopened VA Claims
The VA marks the effective date of a reopened claim as the later of the two dates on which the VA received the reopened claim and the entitlement to the benefits “arose.”
VA cannot use the dates from the original claim in a reopened claim that was finally denied. However, if you are able to prove that the VA made a “clear and unmistakable error,” you can argue to have your effective date changed back to the date your claim was originally filed.
h3 id=”h-effective-date-for-claims-to-increase-ratings”>Effective Date for Claims to Increase Ratings
In some cases, you may be eligible to increase the rating of an already service-connected disability. The effective date that your VA claims benefits are based on is either the date you file the claim to increase your ratings, or the date the disability increased in severity – whichever is later.
h3 id=”h-how-does-the-va-determine-the-true-date-of-a-claim”>How Does the VA Determine the True Date of a Claim?
It is not uncommon for the VA and a veteran (or the veteran’s appointed representative) to end up disagreeing on exactly what the true date is. As in any complex process, the rules that govern what qualifies as a claim for benefits are not always clear cut.
A main reason the VA may not always assign the correct effective date is that claimants often file communications that are not clear. This leads to situations where the VA awards a service connection for a disability using a later effective date than it should.
In this case you may argue that the effective date should be earlier. The VA claims process requires the VA to go back and review your file by freely interpreting all communications. If the VA finds evidence that the claim was made earlier than you thought it was, the VA may owe you retroactive benefits.
h3 id=”h-does-a-form-have-to-be-filed-to-count”>Does a Form Have to Be Filed to Count?
VA policy states that “a specific claim in the form prescribed by the Secretary must be filed in order for benefits to be paid or furnished to any individual under the laws administered by the Secretary.”
Yet there are exceptions and the VA does not have to receive a paper or electronic “form” for every different type of claim.
In cases where the VA does have a form for the veteran to use, the date the VA receives this form is not necessarily the effective date of the claim. Filing a specific form is part of the process to be completed at some point in time. The actual effective date is still established by the date of the original claim, whether it is formal or informal, that the veteran submitted to the VA.
h3 id=”h-what-communications-or-actions-qualify-as-a-va-claim”>What Communications or Actions Qualify as a VA Claim?
Various definitions exist concerning what kinds of communications qualify as VA claims.
Basically any formal or informal communication or action that demonstrates the veteran’s intent to apply for an identified benefit or belief in entitlement qualifies as a claim.
Communication from the veteran’s disability lawyer (if the veteran has given them power of attorney), a Member of Congress, or a minor claimant’s “next friend” would also qualify.
h3 id=”h-oral-communication-as-a-va-claim”>Oral Communication as a VA Claim
Does oral communication between a claimant and a VA employee qualify as an informal claim?
No. According to The Court of Appeals for the Federal Circuit, no oral communication, no matter how specific, will qualify as an official claim because the regulatory definition of a “claim” stipulates that it must be “in writing.”
There are some cases where a VA employee records the veteran’s oral communication on paper. This “Report of Contact” form falls in somewhat of a grey area. The VA states that in certain circumstances, this can qualify as an official informal claim. However, in the case of King v. Shinseki, the panel of judges did not agree that this type of document should qualify.
A situation that does not qualify as an “informal claim” for a service-connected disability is if a veteran seeks treatment at a VA medical center. Just seeking treatment, without following it up with any official VA claims, only indicates intent to apply for treatment.
h3 id=”h-how-are-disputes-over-which-va-claims-qualify-handled”>How Are Disputes Over Which VA Claims Qualify Handled?
Disputes concerning whether a written communication or action qualifies as an informal claim may ensue. This form of dispute is usually solved by answering two key questions:
- Is there an “indication of an intent to apply for one or more benefits?”
- Has the claimant “identified the benefit sought?”
As with most issues, the VA is supposed to err on the side of the veteran when trying to decide if the answers to the above questions have been appropriately provided. This is especially true concerning mental illnesses.
For example, if a veteran has filed a claim for service connection for post-traumatic stress disorder (PTSD), but it is later diagnosed that he actually has a different mental disorder, the VA must still approve the claim as long as certain factors are met. These factors are:
- The claimant’s description of the claim encompasses the newly diagnosed mental disorder
- The claimant’s symptoms apply to the newly diagnosed mental disorder
- The information that the claimant submitted supports his or her VA claims
Chapter 9: Veterans Pension
Veteran’s pension is needs-based welfare. Pensions are paid when any total disability leads to the veteran requiring financial assistance. It does not matter whether the veteran’s disability is service-connected or not. VA pension payments are considerably lower than VA compensation payments.
Pension is only available to certain veterans, such as individuals who served during a period of war or who are totally disabled from any type of work.
Instead of a percentage amount, pensions are paid in a flat amount and are offset by other income dollar-for-dollar. The VA pension program allows for some favorable presumptions. For example, any veteran over the age of 65 is presumed to be totally disabled for the purpose of the pension program. Again, it is not necessary that the disability be service connected.
h3 id=”h-non-service-connected-disability-pension-veterans-benefits”>Non-Service-Connected Disability Pension Veterans Benefits
In certain cases, the VA provides pension benefits to disabled veterans who were made to give up their careers while serving in the military during war time. Now fully disabled, veterans have difficulty supporting themselves and their families.
These payments are designed to compensate for income and resources that these veterans would have accumulated had they not been called to serve their country.
h3 id=”h-non-service-connected-disability-pension-vs-compensation”>Non-Service-Connected Disability Pension vs. Compensation
Non-service-connected pension benefits are based on three important factors:
- The disabled veteran participated in wartime service that eventually led to a discharge under any conditions other than dishonorable.
- The veteran currently has permanent and total disability.
- The veteran has demonstrated need. The VA determines financial need using a calculation that takes into account both the veteran’s income and net worth.
All medical expenses, including the cost of nursing homes, can be deducted from the veteran’s total income. This can be critical as it may help some middle and upper-class veterans show that they are in need of these non-service-connected pension benefits for their standard of medical care.
h3 id=”h-the-five-basic-eligibility-criteria-for-pension”>The Five Basic Eligibility Criteria for Pension
In order to make the VA claims process as straightforward as possible, the Department of Veterans Affairs has established five basic requirements that will be used to determine whether a claimant is eligible to receive the veterans’ benefits of a pension:
- The veteran in question must have been discharged under any condition other than dishonorable.
- Separate rules apply to any veteran who first enlisted in the military on or after September 8, 1980. In these cases, the veteran in question must have completed either 24 months of continuous active duty or the “full period for which the veteran was called or ordered to active duty.”In addition, the veteran must have had at least one of the following:
- A total of 90 days of service during one or more periods of war
- 90 or more consecutive days of service with at least one day coming during a period of war
- At least one day of service during wartime that resulted in a discharge for a service-connected disability
- The veteran must pass the “need test,” which means that you must have a limited net worth and income that doesn’t provide you with adequate maintenance.
- At the time of your application for pension, the veteran must be permanently and totally disabled.
- Willful misconduct must not have led to the veteran’s permanent disability, or you will not qualify for a pension through the current VA claims process.
h3 id=”h-three-different-pension-programs”>Three Different Pension Programs
The three different pension programs in which eligible veterans may be enrolled are
- the Improved Pension Program
- the Section 306 Pension Program
- the Old-Law Pension Program.
Congress establishes a different maximum amount of pension benefits in each of the three pension programs that the VA can pay a veteran.
The program you are eligible for depends on when you applied. The amount of your pension is decided based on disability and need. This is calculated using your countable income, dollar-for-dollar, and net worth. What is left is the monthly veterans’ benefits pension rate.
h3 id=”h-improved-pension-program”>Improved Pension Program
The Improved Pension Program is the only pension program for which new applications can be filed. It came into effect on January 1, 1979.
In this program, all of the income of the veteran, the spouse, and/or any dependents is counted in the VA’s calculation for the veteran’s need. Although this obviously works against the veteran, the calculation is offset by the fact that the Improved Pension Program has a much higher maximum annual pension rate than the other programs.
h3 id=”h-section-306-pension-program”>Section 306 Pension Program
Any veteran who applied for a pension between July 1, 1960, and December 31, 1978, was eligible for the Section 306 Pension Program.
Under this program, the earned income of the veteran’s spouse is almost always added as countable income. The only ways the spouse’s income is not counted is if either the income is not available to the veteran or if counting the spouse’s income would lead to hardship for the veteran.
On January 1, 1979, anyone who was receiving the Section 306 pension was given a choice to either keep that pension or switch to the Improved Pension Program. For those who chose to stay under Section 306, their benefits will be protected but never increased.
To this day, they may still elect to switch to the Improved Program, but once they switch, they are never allowed to switch back.
h3 id=”h-the-old-law-pension-program”>The Old-Law Pension Program
Any veteran who applied for a pension before July 1, 1960, received benefits under the Old-Law Pension Program. The main difference in this program from the other two is that it does not include a spouse’s income when calculating the veteran’s countable income. Also, net worth does not come into consideration when determining need.
Much like the Section 306 Program, anyone who was on the Old-Law Pension Program on January 1, 1979, was given a choice of whether they wanted to switch to the Improved Pension Program.
Again, if they don’t switch, their pension benefits are protected but will never increase. But if they do switch their VA claims to the Improved Pension Program, they can never switch back.
h3 id=”h-what-is-countable-income-as-it-relates-to-pensions”>What Is Countable Income as It Relates to Pensions?
The definition of permanent and total disability, as it relates to the veterans benefits pension rate, has not changed at all over the last 30 years. However, the way the VA counts a veteran’s income for the purposes of calculating their pension amount has changed a great deal.
Basically, any income the veteran receives from any place is considered to be countable; that part has not changed.
The primary changes have come with how the VA counts the income of the veteran’s dependent spouse. While the spouse’s income used to be left out in certain instances, it is now counted fully in the Improved Pension Program.
This change was spurred by the increased presence of women in the workforce. One benefit a veteran gets from having a dependent spouse is that it will increase the maximum annual pension payment that is available to them.
A veteran under today’s VA claims pension rates (effective December 1, 2014) can qualify for a pension of up to $12,868 per year. A veteran with a dependent spouse, on the other hand, can qualify for a pension as large as $16,851 per year.
Another change that came with the Improved Program is the way in which the VA actually counts income. While it used to be counted based on income received within a calendar year, it is now counted on a prospective, annualized basis. This means that the VA will project the veteran’s income for the next 12 months and use that to determine their pension amount.
h3 id=”h-how-va-calculates-veterans-benefits-pension-rate”>How VA Calculates Veterans Benefits Pension Rate
The process for calculating VA pension benefits is a simple one.
First, Congress establishes a maximum amount of pension benefits that the VA can pay a veteran. There are three separate amounts for the three different programs (Improved Pension Program, Section 306 Pension Program, and Old-Law Pension Program).
The VA will then deduct the veteran’s countable income, dollar-for-dollar, from this maximum limit. What they are left with is the monthly veterans’ benefits pension rate.
Chapter 10: Presumptions and Rules in the VA Claims Process
h3 id=”h-favorable-presumptions”>Favorable Presumptions
The VA claims process is known to be problematic for veterans trying to navigate the claims process on their own. Claim denials or too low ratings are very common, and even claims that are finally approved can take years of fights and appeals through the system.
There are a number of presumptions that work together with every claim for benefits from a veteran. Some of these presumptions work to your benefit; others work to your disadvantage.
This portion of the guide outlines the favorable and “helpful” presumptions that veterans enjoy through the claims process.
One critical presumption that can help avoid claim denial is that you entered into your service in good health.
The truth is, you had to pass physical exams before serving your country. If you were not in sound health, you could not have done so. Yet the VA often sidesteps this presumption when arguing that a disabling condition existed prior to a veteran entering the service.
The VA has the burden of proof in this case – it must show through clear and unmistakable evidence that your condition was in fact preexisting.
h3 id=”h-aggravation”>Aggravation
Another presumption working in your favor is that for any preexisting condition that you had treated while you served in the military, that treatment was received because the condition was aggravated by the nature of your service.
In order to deny a claim, the VA must disprove the aggravation presumption with clear evidence. Plus, the VA must show that the original condition got worse due to “natural progress.”
With most conditions, this is not easy to prove because it is powerfully evident that the nature of military service often causes a great deal of physical overuse and damage.
h3 id=”h-agent-orange”>Agent Orange
If you served in Vietnam during the war, VA will presume that you were exposed to Agent Orange. If you develop certain forms of cancer, Type II Diabetes, or numerous other disabling conditions, it will be blamed on Agent Orange and considered to be connected to your service.
h3 id=”h-helpful-rules-for-claimants”>Helpful Rules for Claimants
The time it takes to process a claim is tediously long, often taking over four months. There are so many rules and processes involved, it is easy to miss one or make a mistake, ending in a claim denial for a trivial or preventable reason. And if you try to appeal, you may wait years to get your benefits.
Fortunately there are some helpful rules and laws the VA uses that actually do help you in the claim process. These are “benefit of the doubt,” “duty to assist,” and “lenient standard of proof.”
h3 id=”h-helpful-rule-1-benefit-of-the-doubt”>Helpful Rule 1: Benefit of the Doubt
The Benefit of the Doubt rule is based on a term called “equipoise.” Equipoise means there are two different opinions on something.
For instance, this could mean that one doctor says your impairment is not service connected, while another doctor believes it is. Or it could refer to the fact that an initial medical report labels you as 40-percent disabled, but a follow-up report says you are only 20-percent disabled.
Under Benefit of the Doubt, the VA should always go with the outcome that benefits the veteran more. While Benefit of the Doubt seldom happens, it is certainly very helpful when it does.
h3 id=”h-helpful-rule-2-duty-to-assist”>Helpful Rule 2: Duty to Assist
The Duty to Assist rule works like this: if you file a claim, the VA has a “duty to assist” you in developing the claim. The truth is, the VA was doing such a poor job in this duty that in 2000, Congress passed legislation that redefined what the VA is obligated to do in more explicit terms.
This is the Veterans Claims Assistance Act, and it essentially pressured the VA to better assist veterans.
The two main actions the Act requires the VA to do are:
- Tell veterans what they need to do to prove their claim. The VA must provide documentation to the veteran before the claim is judged on the five specific subject areas the VA uses to determine claims. Failure to do so will cause the VA to be remanded.
- Obtain important records and conduct a thorough examination. It is the VA’s responsibility to get not only your service medical records, but also any related records you tell them about.
h3 id=”h-helpful-rule-3-favorable-standard-of-proof”>Helpful Rule 3: Favorable Standard of Proof
Unlike civil court where proof is determined by a “preponderance of the evidence,” the standard of proof for VA claims favors veterans. To win a claim, a veteran need only show that “as likely as not” his or her current disability resulted from an incident that occurred in the service.
By no means does this infer that it is easy win and avoid getting denied benefits. Doctors’ statements cannot speculate or be unsubstantiated, and must show that all medical records have been taken into account.
h3 id=”h-unfavorable-presumptions-in-the-veterans-claims-process”>Unfavorable Presumptions in the Veterans Claims Process
Just as there are “good” presumptions that serve to help veterans to secure the aid they need from the VA, there are also unfavorable presumptions. These can lead to the VA denying benefits claims, and are explained below.
h3 id=”h-substance-abuse”>Substance Abuse
Smoking, drinking and use of recreational drugs – if it is possible that these behaviors or habits can be tied to your current disabling condition, the VA will likely strive to do so.
For example, you believe your lung cancer is service-connected. You also have been a smoker most of your life. The VA will use all of the evidence it can to show that your current disabling condition is a result of substance abuse and not due to your military service.
h3 id=”h-misconduct”>Misconduct
The VA may try to show that your impairment is the result of some form of misconduct. The argument in a case of misconduct is that your disabling condition did not result from something you were asked to do as a part of your service, even if the actual incident occurred during a period of service.
h3 id=”h-the-presumption-of-regularity”>The Presumption of Regularity
The Presumption of Regularity basically says that government employees generally do the right thing. For example: You claim you did not receive required documentation about your VA claim decision (such as your VA claim is denied, and now you have a limited time to appeal).
The VA can counter with the Presumption of Regularity. This means that even if there is zero proof of the VA mailing the documentation to you, it is presumed that the documentation was sent, and you lose the argument.
The only way a veteran can win in this instance is if the veteran can show that there are records of the paperwork being mailed to the wrong address. The Presumption of Regularity is exceedingly frustrating and sadly happens more than it should.
Read more about how to Obtain Medical Evidence to Support Your Claim.
Chapter 11: Appeal a Denied VA Claim
The Department of Veterans Affairs continues to confront a tremendous backlog of claims. An overwhelmed and undertrained staff continues to be severely challenged to improve the speed and accuracy of decisions.
Many claims are wrongly denied and are appealed and finally overturned, because the claims adjudicators do not understand how the veterans’ claims process works. If your VA claim is denied, it can lead to years of a complicated appeals process.
Consider consulting an accredited VA attorney or agent to help.
h3 id=”h-the-process-of-appeal”>The Process of Appeal
The veterans’ claims process begins at your Regional Office. After a lengthy processing period, a claim adjudicator evaluates your case and determines whether to approve or deny it.
A veteran may also be denied benefits by receiving a 0-percent disability rating. In other words, the VA admits you have a disability, but does not believe you are disabled to the level of being eligible to receive compensation. Or, you may also be assigned a lower disability rating than you believe your situation deserves.
h3 id=”h-three-main-issues-examined-in-a-va-disability-decision”>Three Main Issues Examined in a VA Disability Decision
- Connection of your disability to your service. If the VA determines that your disability is not the result of an event that occurred during service, you will be denied benefits. The VA will not proceed to look into the other two elements if it finds your disability is not connected. To prove a connection, you must point to a specific event during military service that caused your current disability, show that you had no preexisting condition that could have caused it (or that the preexisting condition was aggravated during service), and demonstrate a “nexus” – that the disabling condition is specifically tied to that event that took place during your service.
- Percentage to which you are disabled. VA follows a Schedule for Ratings with a set of diagnostic codes by which they evaluate your level of disability. These codes describe various disabilities and assign percentages to them based on the severity of each condition. A rating officer compares the medical description of your disability to the diagnostic code that most closely matches it, and assigns the percentage to which you are found to be disabled. A 0 percent finding still means that the VA acknowledges the disability is service connected, so you can then appeal the percentage.
- Your effective date. The retroactive date from which the VA has to pay you benefits. Most often, this ends up being the original date that you filed the claim, but in some cases you might even receive retroactive benefits from the date of your injury. Veterans who file claims within a year of being discharged generally receive retroactive benefits from their discharge date. If you eventually win your appeal after years of fighting, you will be paid back from the date of your initial claim. The effective date is a critical component to the claims process, often involving a great deal of money.
If your claim for benefits is denied based on any of these issues, don’t worry – you can appeal.
h3 id=”h-if-your-claim-is-denied-notice-of-disagreement-nod-with-the-regional-office”>If Your Claim Is Denied: Notice of Disagreement (NOD) with the Regional Office
If your claim is initially denied at the VA Regional Office, do not give up! There are a number of things you can still do at the RO level.
Notice of Disagreement: When your claim is denied or an unfairly low rating happens, you have the option to file a Notice of Disagreement (NOD) with the Regional Office up to one year after the rating decision.
Additionally, you have the option to request a hearing before a Decision Review Officer (DRO). This must be preceded by filing a Notice of Disagreement (NOD). In some cases, this is the only time you have the chance to speak with a live person about your VA claim. This hearing is recorded and transcribed. New evidence can be considered for the final decision.
Statement of the Case (SOC): After the VA Regional Office receives your NOD, the VA is required to send you a Statement of the Case. There is no set time in which it must be done.
The SOC lists evidence examined by the VA, adjudicative actions that took place, relevant VA law and regulations, and the justification and basis for the decision. The SOC is sent to both you and your Veteran Service Officer.
If your claim is denied after exhausting your resources at the regional level, your case will move out of the RO and on to the Board of Veterans Appeals.
h3 id=”h-how-to-file-a-formal-appeal-with-the-board-of-veterans-appeals-bva”>How to File a Formal Appeal with the Board of Veterans Appeals (BVA)
The most important thing about receiving the SOC is that you must file a formal appeal within 60 days of the date on the letter – or within one year of the original rating decision for your claim.
The process can be lengthy, and the Board of Veterans Appeals may take up to two and a half years to reach a final decision.
The first step is to send a Formal Appeal to your Regional Office using VA Form 9, Appeal to Board of Veterans’ Appeals. This appeal will be certified and docketed by the Board of Veterans Appeals. You will receive a confirmation from the BVA, as well as a clarification of the appeals process and any estimated delay in considering your case.
You may submit additional evidence before the BVA makes any decision on your claim. This is your opportunity to submit further evidence and information to bolster your VA appeal at a personal hearing.
The BVA hearing can be set up as a video conference or be held at your RO by a Traveling Board Member, or may take place in Washington, DC. You can appear alone, but you can also choose to be represented either by a veteran service officer or an accredited VA disability attorney. The BVA will eventually issue one of three decisions: to deny the claim, remand the claim for further development, or to grant the claim.
h3 id=”h-what-happens-if-the-bva-denies-my-appeals-claim”>What Happens if the BVA Denies My Appeals Claim?
If the BVA denies your appeals claim, you may move up to the second level and file an appeal to the Court of Appeals for Veterans Claims. This second appeal must be filed within 120 days after receiving the BVA’s decision.
It is critical to act fast if you receive a negative decision on your VA claim.
If your case gets to the Court of Appeals for Veterans Claims, do not be disheartened. Yes, the VA claim process can be frustrating and lengthy. Still, tremendous long-term benefits can be gained by appealing a denial!
h3 id=”h-when-should-you-hire-a-va-disability-attorney-after-a-denied-appeal”>When Should You Hire a VA Disability Attorney after a Denied Appeal?
The law states that a veteran must hire an attorney within a year after a negative decision. But more important is that a denied claim has to be appealed by the veteran within 120 days of the VA’s final decision. You must be proactive and retain the attorney and appeal the decision according to the 120 day rule, and disregard the “1-year” window.
In the realm of VA appeals, 120 days is not much time. You need to retain accredited representation as soon as possible.
If a veteran fails to retain legal counsel or representation until after that 120 days, all the vet can do is request the VA to reconsider his or her claim. The VA seldom grants this request. If the VA does comply and reaches the same decision, there is no way for the veteran to appeal the decision.
Repeat: It is critical to act fast if you receive a negative decision on your VA claim.
h3 id=”h-the-adjudication-process”>The Adjudication Process
Four-Step Adjudication Process at the VA Regional Office Level
Regional offices use a four-step process to adjudicate disability claims for any service-connected compensation benefits. Each step is completed before proceeding to the next:
Step 1: The VA decides whether the veteran in question is eligible to receive VA benefits. This includes deciding that the veteran was separated or discharged under any condition other than dishonorable.
Step 2: The VA uses all the rules it has set forth to determine whether the veteran qualifies for disability compensation.
Step 3: The VA determines just how severe the veteran’s disability is, using a percentage evaluation that ranges from 0 to 100. This is based on the Schedule for Rating Disabilities.
Step 4: The VA determines the effective date for the award of the appropriate service-connected disability compensation.
h3 id=”h-duties-of-the-va-in-the-disability-claims-adjudication-process”>Duties of the VA in the Disability Claims Adjudication Process
The VA is obligated to do all it can to aid and assist veterans in developing their claims. These duties are defined in the Veterans Claims Assistance Act of 2000.
The VA has the duty to:
- inform the veteran of all information necessary to complete the claim application
- inform the veteran of all information or evidence (both medical and lay) that will be needed to substantiate any VA claims the claimant has
- inform the veteran of which information will be provided by the secretary and which information needs to be provided by the veteran
- “make reasonable efforts to assist the veteran in obtaining evidence necessary to substantiate the claim”
- “make reasonable efforts to obtain any relevant records” that the veteran authorizes the VA to obtain.
- acquire any of the veteran’s relevant medical records that are held by the Federal government, including: military medical records, other military records, records of VA medical treatment, and any other pertinent records
- acquire a medical opinion or provide a medical examination when one is necessary to make a decision on any disability claims in question
h3 id=”h-adjudicating-a-preexisting-condition”>Adjudicating a Preexisting Condition
When the VA is evaluating whether an injured veteran’s claim is valid, one of the first things an examiner will consider is the veteran’s medical records from the time he or she first entered the service. It may be that the veteran already had a disease or injury before a military career.
This will have been “Noted on Entry into Service” on the veteran’s records and affirmed by the veteran.
h3 id=”h-when-is-a-preexisting-condition-noted-on-entry-into-service-eligible-for-compensation”>When Is a Preexisting Condition Noted on Entry into Service Eligible for Compensation?
Despite being noted on entry, a preexisting condition does not always prevent you from being compensated for those same injuries and diseases you had when you entered into military service.
A preexisting condition is eligible for benefits if you can show the condition was aggravated during service. In these cases, the amount of the compensation will be set at a level that is based on the degree to which the disability worsened after you were enrolled into military service.
Remember: any veteran with a preexisting condition may still be eligible for disability compensation if they are somehow able to get that condition service-connected.
Chapter 12: How to Obtain Medical Evidence to Support Your Claim
Before you undertake a VA compensation claim, it is critical to understand what is involved in obtaining the medical evidence to satisfy the nexus requirement—or linkage evidence. The format is simple – all you generally need is a letter or statement from a doctor/medical expert. This can be your private medical provider or one employed by the VA.
Occasionally the linkage evidence will be provided by way of military medical records or a physician’s in-person testimony.
Just as important as the medical records is the careful wording and thoroughness of the doctor’s statement. The medical opinion connecting a veteran’s disability to a triggering service incident must be based on examination and reasoning, not just the veteran’s testimony, and must specify the rationale used by the physician to arrive at the opinion.
The terms and language of the doctor’s statements should be very clear and specific. Ambiguous or careless phrasing has been a frequent cause of claim denials in past cases.
The VA often rules medical experts’ opinions insufficient if analysis and reasoning are not clearly expressed in the opinion. Always review your medical records when you attend doctor’s appointments, to be sure your physician is very clear in his or her details on your records.
Choosing the right medical expert is also important to obtaining a favorable decision. The expert does not have to be a doctor, but must have some sort of medical training in the field relevant to your medical condition. Feasible experts include doctors, nurses, psychologists, and social workers.
Some medical experts are better than others; choose carefully, and search out highly trained individuals who have a good reputation in your local community.
h3 id=”h-other-strategies-to-remember”>Other Strategies to Remember
You may also submit evidence besides medical opinions to support your claim. This material may include studies and articles found in medical journals. While not sufficient to prove a nexus of evidence, this form of evidence can support your case and influence the VA if a medical opinion is not quite conclusive.
Suppose you do not provide a medical opinion to support your claim. The VA would provide for an examination so that an opinion can be obtained. But first, you need to present to the VA satisfactory evidence that you are disabled, and evidence of an incident during service that could have led to the disability.
Alternatively, if the VA determines that there is no rational way a medical exam would lead to a favorable ruling, it will throw the case out.
The VA can decide to subject you to an additional medical exam administered by a VA physician, in addition to the medical opinion you provided. This generally happens when the VA wants to disprove a case.
If this is your situation, stay the course and work with your appointed representative to make certain that you have provided as much and as strong evidence as possible to fortify your claim.
If your case is denied, you may re-apply for veterans’ benefits. If you need to re-open a claim, be aware that new evidence will be required before the VA will revisit your case. The evidence you will need is going to depend on the reason the VA denied the earlier case.
h3 id=”h-how-to-prove-service-connection-by-aggravation”>How to Prove Service Connection by Aggravation
You can prove service connection by aggravation when explicit evidence in your military medical records indicate that your current disability has gotten worse. Unfortunately, many veterans’ records do not contain such clear-cut proof. If you believe that your service records are not solid enough for the VA, there are other ways to establish the service connection by aggravation.
An alternate method is to bring in a qualified physician or other medical expert to establish the change in severity of your impairment before and after your period of military service. The medical records and testimony provided by hired medical experts along with lay evidence from witnesses who can confirm the change in your disability’s severity, may be enough to win a favorable decision for veterans’ benefits.
h3 id=”h-case-law-regarding-aggravation”>Case Law Regarding Aggravation
During the last few decades, various court cases have considered whether old VA rulings showed “clear and unmistakable error” (CUE) in finding against the veteran. In some cases the VA may be required to prove – by clear and unmistakable evidence – that a veteran’s condition was not aggravated by military service.
Your appointed lawyer may be able to cite past US Court of Appeals for Veterans Claims decisions that support your claim of service connection by aggravation. Case law often has direct bearing on current VA claims. An experienced veteran’s disability lawyer will know to thoroughly review the language in these relevant court decisions.
h3 id=”h-service-connection-by-aggravation-if-disability-was-not-noted-during-entrance-exam”>Service Connection by Aggravation if Disability Was Not Noted During Entrance Exam
Veterans can usually only use the service connection by aggravation if their current disability was observed and noted during their service entrance examinations. But in some cases, even if your disability was not noted during your entrance examination, you may still be able to successfully argue for veterans’ benefits by taking advantage of the fact that the burden of proof is placed entirely on the VA.
Consulting an accredited veterans’ attorney will be key to proving a case that has no entrance exam documentation of your current impairment.
h3 id=”h-service-connection-by-legal-presumption”>Service Connection by Legal Presumption
There are plenty of complex strategies and methods used to successfully argue veterans claims. If your current disability is eligible for service connection by legal presumption, you have reason to be encouraged. This is a very straightforward method through which veterans benefits can be won.
Service connection by legal presumption is often called a “liberalizing rule.” The rule came about because certain veterans were unable to meet the standard of at least 50% proof (or the benefit of the doubt) that their current condition was linked to active service.
For example, if prisoners of war could not document their captivity, they were unable to provide the necessary evidence that showed their current conditions began during periods of captivity. The service connection by legal presumption was created to remove the burden of proof in cases where basic medical principles surpassed the need for a nexus of evidence.
h3 id=”h-requirements-for-va-claims-using-service-connection-by-legal-presumption”>Requirements for VA Claims Using Service Connection by Legal Presumption
To demonstrate a service connection by legal presumption, you must establish diagnosis of a current disability that falls into one of the following categories:
- Tropical diseases acquired during service
- Diseases specifically occurring in former prisoners of war
- Diseases specifically occurring in veterans exposed to radiation during service
- Diseases specifically occurring in veterans exposed to harmful toxins like herbicides (i.e. Agent Orange), mustard gas, or Lewisite during service
- Other diseases pertaining to Gulf War veterans
You must also have served at least 90 consecutive days of active service (NOT including active or inactive training) on or after January 1, 1947, to be eligible for the service connection by legal presumption.
To successfully prove your case, you need to provide evidence that the current disease or injury presented at least a 10-percent degree of disability during the presumptive period specified for that condition.
You will not need to be concerned whether your injury or disease was officially diagnosed during service or during the presumptive period. You just need to be able to prove that symptoms were present during either of those times. Accordingly, the VA then presumes the service connection.
Note: The various eligible diseases each have different presumptive periods. An accredited VA attorney or agent will be able to advise whether your case qualifies for this type of service connection.
h3 id=”h-can-the-va-deny-benefits-in-cases-that-use-the-service-connection-by-legal-presumption”>Can the VA deny benefits in cases that use the service connection by legal presumption?
Yes, but the only way is for the VA to demonstrate “affirmative evidence” that your specific condition occurred during the presumptive period and not because of active service. The aggravation must have been caused by an incident that occurred after discharge or because of your willful misconduct.
If you think that your current condition fits the legal presumption rule but is not exactly stated by the VA on its list of eligible diseases, you may still be able to successfully argue for VA disability benefits. You and a qualified disability attorney can develop a compelling case using medical evidence and private physicians’ statements.
h3 id=”h-using-service-connection-by-legal-presumption-for-chronic-diseases”>Using Service Connection by Legal Presumption for Chronic Diseases
With various specific chronic diseases, the VA automatically presumes the link between the veteran’s disease and the time in service and awards benefits.
The list of chronic conditions allowed for this presumption is very long and includes tuberculosis, Parkinson’s disease, various types of cancer, epilepsy, and many other ailments.
A veteran whose disability is on the VA’s most current list will need to meet the requirement of the presumptive period. To be eligible to use the service connection by legal presumption in a claim, the vet will need to provide medical evidence that the disease manifested to a degree of at least 10 percent within one year after his or her active service ended.
If you were diagnosed and treated with a chronic condition within the presumptive period, your case is fairly straightforward. But take note: if diagnosis took place after the presumptive period, you will need to have sufficient medical evidence to be successful. The most important piece of evidence to provide is a physician’s medical opinion clearly stating that it is as likely as not that your disease first manifested during the presumptive period.
h3 id=”h-using-the-service-connection-by-legal-presumption-for-tropical-diseases”>Using the Service Connection by Legal Presumption for Tropical Diseases
The rules for demonstrating service connection by legal presumption for tropical diseases are much the same as for chronic diseases. The tropical disease being considered in the claim must be on the VA’s approved list.
The list of tropical diseases includes malaria, plague, yellow fever, blackwater fever, cholera, dysentery, and various other diseases specific to military service in tropical regions.
Symptoms of the tropical disease in your case must have been acknowledged within one year after discharge. However, this rule can be relaxed in the cases of certain diseases for which the incubation period is known to be longer than a year. As always, the best strategy is to provide as much medical documentation as possible to support your case.
h3 id=”h-service-connection-by-legal-presumption-for-former-prisoners-of-war”>Service Connection by Legal Presumption for Former Prisoners of War
Claims for benefits submitted by former prisoners of war are given special consideration. The VA presumes that certain conditions are related to time in captivity.
It is basically impossible for former POWs to provide medical documentation from the time of their captivity. Therefore the VA presumes that certain disabilities are linked to this period of their service. The veteran is not required to provide any nexus of evidence, and there is no presumptive period. The current disability may have presented at any time after the former prisoner of war was discharged.
Former prisoners of war are, however, required to provide some medical evidence in order to be eligible to receive veterans’ benefits. As with other types of VA claims, the veteran must provide medical documentation proving that the current condition is at least 10 percent disabling.
The veteran must also prove that (1) he or she spent time as a prisoner of war, and (2) the period of time spent in captivity was comparable to the POW circumstances during previous times of war.
h3 id=”h-which-diseases-make-former-prisoners-of-war-eligible-to-use-the-service-connection-by-legal-presumption”>Which Diseases Make Former Prisoners of War Eligible to Use the Service Connection by Legal Presumption?
The VA’s list of the diseases that qualify for the service connection by legal presumption for former prisoners of war is frequently updated. Eligibility for certain conditions is decided by the length of time in captivity. A former POW must have sustained a minimum of 30 days of captivity for a range of diseases including chronic dysentery, avitaminosis, malnutrition, irritable bowel syndrome, and many other disabilities.
Conditions including psychosis, any anxiety disorder, most heart diseases, stroke, hypertensive vascular diseases, posttraumatic osteoporosis and osteoarthritis (and in some cases frostbite) do NOT require any minimum amount of time in captivity. These conditions merely require that the veteran have been a prisoner of war for some period. The service connection by legal presumption can therefore be easily used to argue veterans claims for former prisoners of war with these disabilities.
The VA often changes the eligibility requirements for some diseases, so be sure to consult an accredited attorney or agent to get the latest information. Also, remember that former POWs are eligible for a variety of other types of VA benefits and programs.
h3 id=”h-service-connection-by-legal-presumption-for-radiogenic-diseases”>Service Connection by Legal Presumption for Radiogenic Diseases
Veterans claims based on a disability caused by exposure to ionizing radiation are challenging. It can be difficult to prove exposure to this type of radiation by meeting the level of evidence usually required for direct service connection eligibility. In an effort to make it accessible for veterans with certain radiogenic diseases to receive benefits, the VA has created a service connection by legal presumption.
If the veteran can prove diagnosis of a qualifying disease, and show time spent in the vicinity of ionizing radiation, the connection between the two will be automatically presumed. The lists of qualifying radiogenic diseases and radiation-risk activities are always changing, so rely on qualified VA legal counsel to know whether your condition is eligible.
Although only the listed diseases are granted the automatic service connection, veterans who can show compelling medical opinions that their non-listed conditions were caused by ionizing radiation may also be able to successfully argue VA claims and receive benefits.
A special procedure exists for veterans to establish a service connection for certain other radiogenic diseases. (This procedure is not a presumptive service connection.) For these diseases, the veteran’s case will be reviewed by several organizations after the Department of Defense provides an estimate of the veteran’s amount of radiation exposure. The VA will consider this and the other opinions to make a service connection decision.
h3 id=”h-amyotrophic-lateral-sclerosis-als-special-service-connection-by-legal-presumption”>Amyotrophic Lateral Sclerosis (ALS) – Special Service Connection by Legal Presumption
Veterans stricken with Amyotrophic Lateral Sclerosis – also known as ALS and Lou Gehrig’s disease – may receive special service connection by legal presumption. This disease attacks veterans more often than civilians for reasons as yet unexplained by medical experts.
An established connection between active service and ALS exists. A veteran diagnosed with the disease at any time after discharge is eligible for the presumptive service connection. The sole requirement is that the veteran served in active duty for at least 90 consecutive days.
h3 id=”h-other-instances-of-the-service-connection-by-legal-presumption”>Other Instances of the Service Connection by Legal Presumption
Along with the many scenarios a veteran can use to argue for service connection by legal presumption in their claims, the VA also presents this option to veterans of three recent conflicts: the Persian Gulf War, Operation Enduring Freedom, and Operation Iraqi Freedom.
Basically, a veteran who served in Southwest Asia after August 2, 1990, is entitled to use the service connection by legal presumption if the disability can be described as a “medically unexplained chronic multi-symptom illness.” Examples of this include chronic fatigue syndrome, fibromyalgia, and irritable bowel syndrome.
Veterans of the Persian Gulf War, Operation Enduring Freedom, and Operation Iraqi Freedom may also be entitled to use the presumptive service connection if their current condition is related to certain infectious diseases. To make certain your service makes you eligible for veterans’ benefits using the legal presumption, consult with an accredited veterans advocate.
h3 id=”h-victims-of-agent-orange-exposure-are-entitled-to-use-the-service-connection-by-legal-presumption”>Victims of Agent Orange Exposure Are Entitled to Use the Service Connection by Legal Presumption
Veterans who are disabled due to exposure to Agent Orange exposure are able to use the service connection by legal presumption when arguing their claims. The VA presumes that all veterans who were stationed anywhere in Vietnam during the war, including on inland waterways, may have been exposed to Agent Orange. Therefore, a veteran needs only to prove that he or she served in Vietnam during this presumptive period and has been diagnosed with a condition related to Agent Orange exposure. The VA will then grant veterans benefits via the service connection by legal presumption.
A qualified veterans’ advocate should have a thorough knowledge of the conditions that the VA believes are connected to Agent Orange, so it is a good idea for veterans to seek legal consultation before embarking on veterans claims.
h3 id=”h-va-compensation-claims-what-is-the-secondary-service-connection”>VA Compensation Claims: What Is the Secondary Service Connection?
If your disabling condition is the result of a service-connected condition, you may also be eligible for benefits by using the secondary service connection to successfully argue your claim for VA compensation.
The secondary service connection can be demonstrated either because a service-connected condition contributed to a veteran’s new disability or because a service-connected condition has aggravated a non-service connected condition.
To spell out what is meant by non-service connected condition, the following are examples of favorable claims made on the basis of the secondary service connection:
- A veteran’s service-connected disability contributes to a diagnosis of depression, so the secondary service connection would apply to the depression.
- A veteran is treated for tuberculosis with a medication that causes hearing loss, so the hearing loss is eligible for the secondary service connection.
- A veteran’s knee is wounded in combat and the wound later leads to lower back pain and hip problems, so the later conditions are eligible for the secondary service connection.
h3 id=”h-how-to-use-the-secondary-service-connection-to-argue-va-compensation-claims”>How to Use the Secondary Service Connection to Argue VA Compensation Claims?
The process for applying the secondary service connection to your claim requires that you develop enough compelling medical evidence to prove the link between the secondary condition and the service-connected disability (or the treatment the veteran received for the service-connected disability).
It is most important to obtain a medical opinion from a private physician stating that the secondary condition was definitely (or at least 50-percent likely) caused or aggravated by the service-connected disability.
The VA ordinarily orders a VA-approved medical examination; however, it can be wise to also have a private physician’s opinion to offer as supporting evidence. You can never be too thorough in developing the evidence for your case for VA compensation claims.
h3 id=”h-are-conditions-related-to-tobacco-use-eligible-for-va-claims”>Are Conditions Related to Tobacco Use Eligible for VA Claims?
Veterans may not claim a service connection for any conditions caused by tobacco use during periods of military service. Under no circumstances can tobacco consumption by any method be used in the nexus of evidence for VA claims. This rule also applies to survivors seeking benefits after a veteran has passed away due to a tobacco-related illness.
Now, this restriction is not quite as rigid as it sounds. Granted, the VA cannot award a service connection for conditions that depend on tobacco use to prove linkage. However, a veteran may be able to receive benefits for tobacco-related conditions through other strategies.
h3 id=”h-getting-around-the-tobacco-use-restriction”>Getting Around the Tobacco Use Restriction
It may be feasible to get a favorable decision when tobacco use is involved, IF your disability could be eligible for a service presumption for which you do not need to prove a nexus of evidence—such as the service connection by legal presumption. This depends on whether it is possible to make your case without a private medical expert’s opinion.
Example: If you can use the service connection by legal presumption for a diagnosis of lung cancer due to Agent Orange exposure, you would not be required to provide a physician’s opinion. In this situation it is possible to work the system to secure benefits even if your doctor believes 100% that the lung cancer is the result smoking.
In rare cases, it is also possible to use a loophole in VA policy concerning the use of secondary service connection for conditions caused by using tobacco. If a veteran took up smoking to calm the symptoms of a service-connected ailment (such as PTSD or another anxiety disorder) and then developed a disease because of the tobacco use, the veteran may be eligible for benefits.
The case may be decided in the veteran’s favor as long as he or she can prove the following:
- The condition that caused the tobacco use was service-connected
- The use of tobacco products was a major cause of the secondary disability
- The secondary disability wouldn’t have manifested had it not been for the use of tobacco products
Chapter 13: Family Benefits
Veterans benefits may be granted to certain members of an injured veteran’s family. These benefits may be available to dependents of a living veteran who is unable to support them, or to surviving family members of a deceased veteran.
Benefits for which family members may be eligible include:
- Death compensation
- Death pension
- Accrued benefits, and
- Dependency and Indemnity Compensation (DIC).
The dependents and survivors do not have entitlement rights to the disability claims. Any benefits received by family member are based entirely on their qualifying family relationship to the injured or deceased veteran.
Access to these benefits will depend on the circumstances of the veteran’s service, as well as the veteran’s relationship to the surviving family members.
h3 id=”h-who-qualifies-for-family-member-benefits”>Who Qualifies for Family Member Benefits?
Generally, the following family members can qualify for veterans benefits:
Spouse: To qualify, the marriage must be valid and the surviving spouse must be able to show proof of a legal marriage. Veterans benefits may be awarded to a current spouse in instances where a living veteran is unable to provide enough support for a spouse who is in need, as well as a surviving spouse in the unfortunate situation where a veteran has passed away.
A spouse is only eligible for special allowance benefits if the veteran has been rated at least 30 percent disabled. Also, a spouse can only receive special allowance veterans benefits directly if the veteran is deemed incompetent or is deceased. In all other cases, the veteran collects the funds on behalf of the spouse.
Child: To qualify for benefits, a current child or a surviving child of a deceased veteran must be the veteran’s biological child, adopted child, or stepchild. The child also must: be unmarried, either under 18 years old or between 18-23 and pursuing an education, or be permanently incapable of self-support.
Parent: In order for a dependent parent or a surviving parent to qualify for veterans disability benefits, the parent must show that either his or her financial dependency (in cases of a living veteran) or income eligibility (in cases of a deceased veteran) is reliant on the injured veteran.
h3 id=”h-what-veterans-benefits-are-available-to-qualifying-family-members-of-a-deceased-veteran”>What Veterans Benefits Are Available to Qualifying Family Members of a Deceased Veteran?
Some of the more basic benefits a family member may receive are:
- If the deceased veteran was receiving either a VA pension or VA disability compensation, the surviving spouse may be given the veterans benefits during the month that the veteran died.
- If the deceased veteran was found to have a service-connected condition, the survivors will be eligible to receive a certain amount toward the veteran’s burial and funeral expenses.
- Other veterans’ benefits such as VA health care, VA home loans, and VA educational benefits may be available to surviving family members.
More substantial benefits may be accessible to certain surviving family members of a deceased veteran, including:
- If the veteran filed VA claims when he or she was still alive, certain surviving family members could be entitled to some lump-sum or accrued benefits.
- In the case of certain service-connected deaths, spouses and children may be given a special survivor’s benefit (REPS).
- In some cases, survivors will be given access to monthly VA benefits such as DIC or the death pension.
h3 id=”h-death-benefits-based-on-a-service-connected-condition”>Death Benefits Based on a Service-Connected Condition
In some cases, surviving family members of a deceased veteran may be able to file VA compensation claims to obtain death benefits. To be eligible, service connection must be shown for the disease, disability, or injury that caused or contributed to the veteran’s death. In this situation, the surviving family member will qualify to receive DIC.
h3 id=”h-how-do-you-show-that-a-condition-is-eligible-for-va-compensation-claims-for-death-benefits”>How Do You Show That a Condition Is Eligible for VA Compensation Claims for Death Benefits?
Generally it will suffice for a service-connected disability to be listed on the death certificate as the primary cause of death, as sufficient evidence for surviving family members to receive death benefits.
When the service-connected disability is not the primary cause of death, the family will need to prove that it was at least a contributory cause of death, which would still qualify them for DIC.
The following rules to help clarify whether a service-connected disability might be considered a contributory cause of death.
- The service-connected disability must have contributed “substantially or materially” to the veteran’s death, thereby contributing to the actual cause of death. It is not enough to show that the disability was casually involved in the death.
- Minor service-connected disabilities are normally not considered to have contributed to a death that occurred mostly due to a different disability. This includes most disabilities that were not progressive or did not affect a vital organ.
- Any service-connected disabilities that actively affected vital organs may be considered contributory, even if the primary cause of death was unrelated.
h3 id=”h-death-in-service-how-it-affects-a-family-s-va-claim-for-death-benefits”>Death in Service – How It Affects a Family’s VA Claim for Death Benefits
A death is almost always considered service-connected if a veteran dies while still in service. This includes situations where the soldier has gone missing in action, because his or her death is presumed.
However, some situations happen where a veteran’s death in service is not automatically assumed to be service related. These are: suicide, death by disease within the first six months of active service, and any death that is thought to have come as a result of the veteran’s misconduct.
In these cases, a formal ratings decision will be issued to determine whether the death will be considered service connected, thereby making it eligible for the surviving family members to file VA compensation claims for death benefits.
h3 id=”h-special-survivors-veterans-benefits-the-restored-entitlement-program-for-survivors-reps”>Special Survivors Veterans Benefits: The Restored Entitlement Program for Survivors (REPS)
The Restored Entitlement Program for Survivors (REPS) was put in place in 1983 to restore Social Security benefit payments to surviving spouses and children who should have been entitled to veterans’ benefits. REPS is funded by the Department of Defense (DOD) and administered by the VA. Eligibility factors are a mix of VA and Social Security Administration criteria.
REPS benefits are paid to eligible surviving spouses and children of soldiers
- who were killed in active duty before August 13, 1981, or
- who died of a service-connected disability that began before August 13, 1981.
h3 id=”h-which-surviving-spouses-are-eligible-for-reps”>Which Surviving Spouses Are Eligible for REPS?
A surviving spouse is eligible for REPS benefits if the spouse cares for a child of the deceased veteran while the child is between ages 16 and 18. When Social Security payments stop once the child hits 16, the REPS benefits kick in. In this case, VA compensation claims should not even need to be filed.
If the child is found mentally incompetent, the Social Security payments will usually continue past age 16. In this case, the spouse will receive REPS payments in an amount that will cover the difference between the Social Security payments and what the full REPS payment amount would be. If the spouse remarries, the REPS benefits will terminate. These benefits will, however, be restored if that marriage ever ends.
h3 id=”h-which-surviving-children-are-entitled-to-reps”>Which Surviving Children Are Entitled to REPS?
A veteran’s surviving child is only eligible for REPS benefits in one specific instance: he or she must be between the ages of 18 and 22 and enrolled full time in an approved postsecondary school. The child also cannot be married.
Unlike in the case of a spouse, if a child loses eligibility to REPS veterans benefits for any reason, the child may not reestablish it with VA compensation claims.
h3 id=”h-how-does-income-affect-reps-payments”>How Does Income Affect REPS Payments?
The amount of the benefit is based on information provided by the Social Security Administration. Basically, whatever REPS benefits an eligible surviving family member is entitled to are reduced by $1 for every $2 earned in wages over the designated annual limit. Also, if the survivor is eligible for Social Security, payments will only be made in an amount that covers the difference between what the Social Security payments are and what the REPS veterans’ benefits should be.
h3 id=”h-non-service-connected-veterans-benefits-what-is-a-death-pension”>Non-Service-Connected Veterans Benefits: What Is a Death Pension?
The spouse of a non-service-connected veteran who has passed away may still be eligible to receive monthly veterans benefits in the form of a death pension. This pension is available to qualified spouses in cases where the veteran served at least 90 days of active duty, was discharged under any conditions other than dishonorable, and served at least one day of active duty during a period of war.
If the veteran served after September 7, 1980, in most cases the veteran also must have been in continuous active duty for at least 24 months in order for a spouse to submit VA claims and qualify for the death pension. Exceptions to this 24 month rule are:
- The veteran served the full period in which he or she was ordered to active duty
- The veteran did not serve the full period only because he or she was granted either early discharge or a hardship discharge
- The veteran was discharged or released from active duty because he or she suffered a disability
- At the time of death, the veteran was eligible to receive some form of compensation for a service-connected disability that occurred during wartime.
h3 id=”h-what-is-the-improved-pension-program”>What is the Improved Pension Program?
The improved pension program will be used for any new death pension VA claims filed for by a qualifying survivor. This program bases the awarded pension amount on the survivor’s monetary need by taking into account any current income and measurable assets (not including home value). In some cases, this can lead to a qualifying survivor receiving no death pension at all.
There are some very stringent rules that govern benefit amounts. There are also some rules that govern whether a surviving spouse is qualified to receive the death pension.
If the surviving spouse was married to the veteran for at least one year before death or if a person has a child with the deceased veteran, the spouse or co-parent qualifies. In cases where the surviving spouse married the veteran after discharge, he or she may still be eligible to file VA claims for the death pension if the couple was married prior to these dates:
- Mexican Border Period and WWI: They were married before December 14, 1944
- WWII: They were married before January 1, 1957
- Korea: They were married before February 1, 1965
- Vietnam: They were married before May 8, 1985
- Persian Gulf War: They were married before January 1, 2001
h3 id=”h-the-surviving-child”>The Surviving Child
In most cases, the surviving child of a veteran does not have independent entitlement to the improved death pension if the child is in custody of an eligible surviving spouse. However, the spouse will be able to qualify for more monthly veterans benefits in order to take care of the dependent child.
If the child is not in custody of the surviving spouse, the death pension veterans’ benefits may be paid to the child’s legal guardian.
h3 id=”h-are-there-special-allowances-for-family-members”>Are there Special Allowances for Family Members?
With regards to distributing veterans benefits to family members, the VA has a few special rules to assist and benefit loved ones who need extra assistance. The special allowances fall into two categories:
- family members who require Aid and Attendance (A&A)
- family members who do not need constant supervision but are still permanently housebound (HB).
Both allowance categories are available only to family members who qualify as one of the following in relation to the veteran: a spouse, a surviving spouse, a parent, or a surviving parent.
h3 id=”h-how-can-family-members-qualify-for-special-allowance-veterans-benefits”>How Can Family Members Qualify for Special Allowance Veterans Benefits?
If a veteran’s family member needs daily care and assistance, he or she will meet eligibility requirements for the Aid and Attendance (A&A) special allowance benefit only if one of the following criteria is met:
- Documentation that the family member is blind or nearly blind
- Proof that the family member is in a nursing home due to physical or mental limitations
- Medical evidence or a doctor’s statement that the family member is unable to care for himself or herself and/or protect himself or herself from daily hazards
If a family member’s disability does not fall into any of the above categories, he or she may be able to qualify for the HB (housebound) allowance if it can be proved that the individual is “substantially confined” to the home and will be for the rest of his or her lifetime.
h3 id=”h-va-benefits-for-children-born-with-birth-defects-in-the-vietnam-war-era”>VA Benefits for Children Born with Birth Defects in the Vietnam War Era
Under the Agent Orange Benefits Act of 1996, children with Spina Bifida born to Vietnam veterans are ruled eligible to receive increased veterans benefits that include health care coverage, vocational rehabilitation in the case that the child is capable of holding down a job, and a monetary allowance that is adjusted yearly to compensate for increased cost-of-living.
The children of female veterans who served in Vietnam during the dictated time period that exhibit birth defects other than Spina Bifida may also be eligible for additional benefits. A qualified disability attorney can help you determine which birth defects make a child entitled to this increased compensation.
h3 id=”h-spina-bifida-what-requirements-must-be-met-to-receive-increased-veterans-benefits”>Spina Bifida: What Requirements Must Be Met to Receive Increased Veterans Benefits?
The VA makes some important distinctions that determine who is eligible to receive additional compensation due to cases of Spina Bifida.
- The child in question must be the biological offspring of a Vietnam War veteran who served between January 9, 1962, and May 7, 1975.
- The child must also have been conceived after the veteran spent some amount of time in Vietnam.
h3 id=”h-how-to-claim-veterans-benefits-for-children-with-spina-bifida”>How to Claim Veterans Benefits for Children with Spina Bifida
Beginning the disability claims process for children with Spina Bifida is fairly easy. The first step is simply to file an informal claim stating that the child has the disability and is eligible under the requirements stated above. Then, you’ll need to submit VA Form 21-0304.
Unlike most disability claims applications, this process does not require the child to be formally examined by the VA. One exception is in cases where the diagnosis is doubted. Because the VA’s decision is made solely on the basis of a doctor’s statement, it is important to retain counsel who can advocate on your behalf and ensure that all medical documentation describes your child’s symptoms honestly and in great detail.
The VA will rate your child’s Spina Bifida across four levels of disability and pay benefits out in accordance with the judgment of severity. Because of this, and because this is a rare circumstance in which the child – not the veteran – files the disability claim, it is important to consult a qualified representative to ensure that you and your son or daughter receive the veterans benefits to which your family is entitled.
h3 id=”h-dic-benefits-for-surviving-family-of-veterans-exposed-to-agent-orange”>DIC Benefits for Surviving Family of Veterans Exposed to Agent Orange
For many years, the VA denied that exposure to the spraying of the chemical Agent Orange during Vietnam could cause any serious diseases or deaths. Veterans were therefore not able to file disability claims for any conditions related to the spraying. This resulted in thousands of qualified surviving family members of deceased veterans being denied benefits that they deserved.
h3 id=”h-how-disability-claims-for-agent-orange-cases-changed-in-the-90s”>How Disability Claims for Agent Orange Cases Changed in the 90s
In the 1990s, the VA changed its position on Agent Orange by admitting that certain diseases could be caused by exposure to the chemical. Because of this change in policy, the VA now must pay out previously denied veterans benefits to the qualified families of those soldiers who died from related diseases.
Thousands more are entitled to these benefits and just need to apply. Many also may be eligible to receive back compensation to make up for the money that the veteran should have been paid when he or she was still alive.
The law presumes that anyone who served in Vietnam was exposed to the chemical.
The surviving family member does not need to prove that the veteran was exposed to Agent Orange to make disability claims. The surviving family must just be able to show that the deceased veteran was diagnosed with a disease that is linked to Agent Orange exposure. This could be as simple as sending the VA a copy of the death certificate that lists an Agent Orange-related disease as one of the causes of death.
Even if one of the related diseases is not listed as the cause of death, a family member can still use a doctor’s opinion to prove that it might have been. That would be enough evidence to receive the deceased veteran’s DIC disability claims benefits.
Chapter 14: Psychological & Cognitive Disabilities
h3 id=”h-disability-compensation-for-mental-disabilities-other-than-ptsd”>Disability Compensation for Mental Disabilities Other Than PTSD
If your case concerns a mental disorder, various unique issues may be present during the claim process. First you must be sure to have your mental disability professionally diagnosed. Once diagnosed, you will need to identify which particular mental disorder you are seeking benefits for; you will also need to show that the disability is service-connected in one of five different ways.
h3 id=”h-the-5-ways-to-service-connect-a-mental-disorder-in-a-va-claim”>The 5 Ways to Service Connect a Mental Disorder in a VA Claim
- The mental disorder that the veteran is suffering from was first evidenced during service.
- The veteran had a preexisting mental disorder that was aggravated by service.
- The mental disorder in question developed soon after a service-connected physical disorder was incurred.
- The mental disorder was diagnosed within a year after service ended. This period of time is extended in any case involving a prisoner of war.
- The mental disorder resulted from an injury that occurred while the veteran was being administered VA medical care.
Disability claims involving mental disorders can be extremely challenging, and more than one mental disorder can exist.
Note: if you have applied for the wrong mental disorder, that alone is not basis for denial. As long as some of the symptoms overlap, the claim can be applied to the correct disorder once it has been diagnosed. You may be required to provide new evidence in the case.
You can receive a separate service connection for each of the different disorders sustained. But – only one disability rating will be assigned to cover any disorders with overlapping symptoms.
h3 id=”h-glossary-of-key-terms-used-in-mental-disorder-va-claims”>Glossary of Key Terms Used in Mental Disorder VA Claims
The VA uses specific language when dealing with veterans claims regarding mental disorders. Common terms are:
Amnestic: Causing loss of memory
Axis: One of the 5 different types of problems a person making VA claims for a mental disorder may have
Axis I: Clinical disorders
Axis II: Personality Disorders and Mental Retardation
Axis III: General Medical Conditions
Axis IV: Psychological and Environmental Problems
Axis V: Global Assessment of Functioning
Bipolar Disorder: A mood disorder where both excitable (manic) and depressed (depressive) episodes take place
Cognitive: The process of thinking
Dementia: A disorder that causes general loss of intellectual abilities and impairment of judgment, memory, and abstract thinking
Dissociative Disorders: Mental disorders such as multiple personality disorder which cause sudden, temporary changes in memory, identity, or consciousness
DSM (III, III-R, or IV): The Diagnostic and Statistical Manual of Mental Disorders. These are previous editions of a reference book developed by the American Psychiatric Association (APA) that classifies known mental illnesses and their symptoms. Although superseded by edition DSM-5 (listed below) the transition from DSM-IV to DSM-5 is still ongoing, and many documents still reference past versions of the manual.
DSM-5: The Fifth Edition of Diagnostic and Statistical Manual of Mental Disorders, developed by the American Psychiatric Association (APA), is the latest compendium of mental disorder criteria and diagnostic codes used by clinicians in the U.S. healthcare system. Released in May 2013, DSM-5 drops the Roman numeral nomenclature and marks the first major revision to the classification of and diagnostic criteria for mental disorders since DSM-IV was released in 1994.
Dysthymic Disorder: A mood disorder that results in depressed feelings and lack of interest in usual activities, but isn’t severe enough to be Major Depression
Personality Disorder: A pattern of behavior that departs from normal cultural expectations. This usually begins during adolescence or early adulthood
Psychotic Disorders: Disorders such as Schizophrenia that result in the afflicted individual having regular delusions or hallucinations that put them out of touch with reality
Psychoneurotic Disorders: A disorder that results in phobias, obsessions, and anxiety attacks. One example of this is Posttraumatic stress disorder
PTSD (Posttraumatic stress disorder): A disorder in which the afflicted person re-experiences an extremely traumatic event. This usually results in nightmares, difficulty sleeping, anxiety attacks, and increased arousal.
Schizoaffective Disorder: A mental disorder characterized by the presence of both schizophrenia and mood disturbances such as depression
Schizophrenia: A disorder where the afflicted are out of touch with reality most of the time. They suffer from grossly disorganized behavior, disorganized speech, delusions, hallucinations, and inappropriate affect.
Somatoform Disorders: A disorder where a person has certain physical symptoms of a medical condition, but tests do not reveal that they actually have that condition
Superimpose: To lay or place something on or over something else
When dealing with cases involving VA claims, it is imperative that your VA disability attorney knows and comprehends the preceding list of terms so that he or she can effectively represent you.
h3 id=”h-eight-categories-of-mental-disorders-eligible-for-va-compensation-claims”>Eight Categories of Mental Disorders Eligible for VA Compensation Claims
Mental disorders are a truly awful thing for anyone to have to live with, but establishing a mental disorder as service-connected can certainly make things somewhat easier by giving the veteran access to care.
To qualify for benefits for psychological and cognitive disabilities, the disorder in question must first fall into certain specific categories.
- Schizophrenia and Other Psychotic Disorders
- Delirium, Dementia, and Amnestic and Other Cognitive Disorders
- Anxiety Disorders
- Dissociative Disorders
- Somatoform Disorders
- Mood Disorders
- Chronic Adjustment Disorder
- Eating Disorder
Any of the disorders included in the eight categories may be eligible for VA compensation claims, depending on whether or not it is determined to be service connected:
Schizophrenia and Other Psychotic Disorders. This category includes any mental disorder that causes loss of contact with reality and derangement of one’s personality. Some of these are schizophrenia, shared psychotic disorder, delusional disorder, and brief psychotic disorder.
Delirium, Dementia, and Amnestic and Other Cognitive Disorders are brain-related disorders that include Alzheimer’s, alcoholism, dementia due to infection, brain trauma, and drug or poison intoxication.
Anxiety Disorders include matters like Post Traumatic Stress Disorder (PTSD), obsessive-compulsive disorder, panic disorder, phobic disorder, and agoraphobia.
Dissociative Disorders can include multiple personality disorder, dissociative fugue, dissociative amnesia, and depersonalization disorder.
Somatoform Disorders are issues such as pain disorder, somatization disorder, conversion disorder, and hypochondriasis.
Mood Disorders may be bipolar disorder, major depression, dysthymic disorder, and cyclothymic disorder.
Chronic Adjustment Disorder involves the inability of the inflicted party to readjust to normal society over a long period of time. It can cause symptoms like anxiety, head and stomachaches, and depression.
Eating Disorder includes both anorexia and bulimia.
h3 id=”h-linking-a-mental-disorder-to-military-service”>Linking a Mental Disorder to Military Service
To qualify for compensation for a mental disorder, you first must prove through the VA claims process that the disorder is somehow related to your military service. This is not always a simple thing to do.
Diagnosis: before filing a claim for a mental disorder, first you must obtain a diagnosis of the condition. The exam should be conducted by a true expert in the field, such as a physician, psychiatrist, or psychologist.
Linkage Evidence: Once diagnosed, evidence must be presented that will prove that the disorder was either incurred during military service, or at the very least aggravated by it. This is usually best done by obtaining a doctor’s expert opinion stating that your mental disorder was either caused by or exacerbated by their military service. A good opportunity to get this sort of expert opinion is during the DSM-5 axis diagnosis. If the examiner includes military service as a factor in the diagnosis, it means the examiner found it to be a clear contribution to the patient’s mental disorder. This can then be used during the VA claims process as evidence to connect your disorder to your service.
h3 id=”h-evaluate-the-degree-of-disability-of-a-mental-disorder”>Evaluate the Degree of Disability of a Mental Disorder
Diagnosing a mental impairment and linking it to a veteran’s military service is the first step.
The next step should establish how severe the impairment is. The VA uses a sliding scale called the “General Rating Formula for Mental Disorders.” This formula measures just how impaired the veteran’s social and occupational functioning are.
The scale focuses specifically on how a veteran’s symptoms affect his or her life. The outcome of this test is then used to determine the extent of the VA compensation claims.
h3 id=”h-criteria-used-to-determine-mental-disorders”>Criteria Used to Determine Mental Disorders
The “General Rating Formula for Mental Disorders” is measured in percentages of disability based on the veteran’s level of impairment.
100 Percent Total Social and Occupational Impairment
Symptoms include persistent delusions or hallucinations, grossly impaired communication or thought processes, disorientation, memory loss for things that should be familiar, persistent danger of hurting self or others, and intermittent inability to perform normal daily activities.
70 Percent Social and Occupational Impairment
This results in deficiencies in thinking, mood, family relations, work, school, and judgment. Symptoms include intermittently illogical speech, suicidal ideation, near-continuous depression or panic that affects the ability to function, obsessed rituals which interfere with the daily routine, unprovoked irritability with occasional violence, neglect of appearance and hygiene, inability to maintain relationships, and spatial disorientation.
50 Percent Social and Occupational Impairment
This will result in reduced reliability and productivity. Symptoms include panic attacks more than once per week, circumstantial or stereotyped speech, difficulty comprehending complex commands, flattened affect, memory impairment, impaired abstract thinking, impaired judgment, difficulty with work and social relationships, and disturbances of motivation and mood.
30 Percent Social and Occupational Impairment
This is marked by an occasional decrease in work efficiency. Routine behavior, conversation, and self-care generally remain normal. Symptoms include anxiety, depression, panic attacks once per week or less, suspiciousness, mild memory loss, and chronic sleep impairment.
10 Percent Social and Occupational Impairment
Symptoms here are mild and result in a decreased ability to perform occupational tasks during periods of high stress. This can be controlled by medication.
0 Percent Social and Occupational Impairment
A mental condition has been diagnosed, but the symptoms are not severe enough to affect social or occupational functioning.
By using the sliding scale (General Rating Formula for Mental Disorders) when processing the claim, the appropriate amount of VA compensation claims can be accurately determined for any veteran who suffers from a service-induced mental disorder.
h3 id=”h-how-a-soldier-with-traumatic-brain-injuries-can-avoid-a-veterans-claim-denial”>How a Soldier with Traumatic Brain Injuries Can Avoid a Veterans Claim Denial
In recent years, the importance of soldiers having their brain injuries correctly evaluated in order to avoid denial of veterans claims has become a hot button topic. One of the main reasons is because of the steep increase in traumatic brain injuries (TBI) suffered by soldiers during our most recent wars. This increase can be linked directly back to an uptick in the use of roadside improvised explosive devices (IEDs) that often cause head trauma after a blast. This can result in posttraumatic stress disorder and depression for those veterans who have been inflicted with these horrible brain injuries.
The significantly higher levels of TBI have led the VA to revise the criteria used to determine the true effects of brain trauma on those who are applying for disability.
h3 id=”h-evaluating-traumatic-brain-injuries-correctly-to-avoid-claim-denial”>Evaluating Traumatic Brain Injuries Correctly to Avoid Claim Denial
Any veteran who may be feeling the effects of a traumatic brain injury suffered during service should immediately see a professional. Also be certain to claim a service connection for any mental condition that may be associated with an injury. This includes both PTSD and depression.
It is also important that you obtain a professional opinion on the ability to be regularly employed. The evaluation should include a “Global Assessment of Functioning (GAF)” score, which is a 0 through 100 rating by a mental health doctor that measures how well you can adapt to and handle various problems that might be encountered in social or work life.
If you are proactive in following these steps, it will make you significantly less likely to be the victim of a denial of veterans benefits.
h3 id=”h-who-is-eligible-for-ptsd-disability-claims”>Who Is Eligible for PTSD Disability Claims?
The criteria for a diagnosis of PTSD are fairly varied, but in general, most returning veterans experience some of the following symptoms:
- Emotional numbness for a long period after the traumatic event
- Survivor’s guilt
- Nightmares about and flashbacks to the traumatic event
- Difficulty sleeping and concentrating
- Strong reactions to sounds mimicking the traumatic event
- Difficulty reconnecting emotionally with friends and family
- Generalized anxiety, nervousness, or depression
The service men and women who put their lives on the line for this country deserve healing through competent and compassionate mental healthcare. If you are a veteran experiencing one or more of these symptoms, you may be eligible for veterans benefits on the basis of a PTSD diagnosis. Do not hesitate to put together a case. Consider contacting an experienced VA disability attorney to help your case make it to the review board.
h3 id=”h-the-three-qualification-requirements-for-ptsd-disability-claims”>The Three Qualification Requirements for PTSD Disability Claims
The VA has policy and standards in place to determine the validity of PTSD-related disability claims.
PTSD Disability Claim: Requirement #1
The most important qualification is a medical diagnosis of posttraumatic stress disorder. The diagnosing doctor must be in good standing with the VA and must strictly adhere to the criteria set out in the DSM-5 when making the determination. If the VA rejects your initial claim, your medical report will be returned for clarification. In some cases, the VA will conduct an independent medical inquiry.
However, because PTSD diagnoses are so subjective, all you need for a positive determination is 50-percent surety on the part of your doctor. Also referred to as an “as likely as not” decision, this makes it easier on the veteran to gain the necessary PTSD diagnosis.
PTSD Disability Claim: Requirement #2
Once the claims process begins, veterans must provide evidence of a stressful event that occurred during military service. The incident did not have to take place during combat.
If your PTSD diagnosis was made during service, the only evidence the second step requires is a personal account of the traumatic event or events that led to the diagnosis. Unless there is clear evidence your personal statement is false, the VA will accept the story as sufficient evidence that the event occurred.
The requirements are slightly different if your PTSD diagnosis occurred after service. In this case, the circumstances of the trauma make all the difference:
- If the stressor occurred during combat, your personal statement is the only evidence necessary to satisfy this step;
- if the stressor is related to a persistent and debilitating fear of hostile military or terrorist activity, again the only evidence necessary is your story, along with a psychiatrist’s evaluation;
- if the stressor is related to an in-service personal assault, you may need to present evidence outside military records to substantiate the claim;
- If the stressor occurred under other circumstances, you may also need to present additional evidence.
PTSD Disability Claim: Requirement #3
If you have successfully provided a medical diagnosis of PTSD as well as a valid stress event, the final step before receiving your rightful disability claim will be to prove the service connection between the diagnosis and the stressor.
This will not be a problem in most cases as the medical records proving the diagnosis will contain details about the stressor claimed in Step Two of the process.
h3 id=”h-special-va-compensation-claims-rules-on-service-connection-for-ptsd”>Special VA Compensation Claims Rules on Service Connection for PTSD
Variations may apply to VA compensation cases for PTSD. In the case of Pentecost v. Principi, the Court of Appeals for Veterans Claims established that a service connection for PTSD requires:
- A current PTSD diagnosis
- Credible supporting evidence that shows that the claimed in-service stressor actually occurred
- Medical evidence that shows a causal connection between the current set of symptoms and the claimed in-service stressor
Proving a claim of PTSD requires much less evidence with a combat veteran than it would with a non-combat veteran, just like with any other illness or injury that is claimed.
In 2008, there was an amendment made to reflect that both combat and non-combat veterans should be given an easier path to establishing the occurrence of their in-service PTSD stressors. This amendment now allows veterans to prove an in-service occurrence of PTSD with lay evidence alone.
Consequently the combat veteran’s lay testimony will generally be all that is needed to establish that an in-service stressor actually occurred. This only affects veterans who were actually diagnosed with PTSD while they were still in service. If their PTSD didn’t appear until after service, the normal service connection rules for VA compensation claims apply.
Chapter 15: Special Rules for Combat Veterans
Combat veterans are apt to have a less difficult time getting their condition service-connected than non-combat veterans. VA law makes it much easier for combat veterans to prove that their disability occurred or was aggravated during service. This reduces the chances that the combat vet is denied VA compensation benefits.
This means a combat veteran does not need to show facts to prove that their disability stemmed from a service-related incident. They just have to make a claim that shows to be consistent with the circumstances and conditions in which they were deployed.
In most cases, the combat veteran’s statement that the disability occurred from a combat incident will be considered as fact. This can only be disputed if someone provides “clear and convincing evidence to the contrary.” (38 C.F.R. §3.304 – Direct service connection; wartime and peacetime.)
h3 id=”h-why-do-combat-veterans-receive-special-treatment-on-va-compensation-claims”>Why Do Combat Veterans Receive Special Treatment on VA Compensation Claims?
This treatment is not due to favoritism or partiality. The reason combat veterans are treated differently is that during combat, military record-keeping can be very disorganized or faulty. Records are easily destroyed or are incomplete, and in some cases, no records exist at all. Because of this, the VA has chosen to err on the side of the combat veteran with regards to compensation claims.
h3 id=”h-what-do-combat-veterans-need-to-prove-to-get-va-compensation-claims-approved”>What Do Combat Veterans Need to Prove to Get VA Compensation Claims Approved?
Combat veterans must still prove the other two service connection requirements in order to receive a favorable decision. Therefore, the combat veteran will need to provide sufficient evidence that he or she currently has a disability along with sufficient evidence that connects the current disability to the in-service event.
h3 id=”h-how-do-you-know-if-an-incident-occurred-while-engaged-in-combat”>How Do You Know If an Incident Occurred While “Engaged In Combat?”
It is absolutely critical that the VA accurately determines whether the event happened while the veteran was “engaged in combat with the enemy.” But how do they make this determination?
Proving that an injury or illness occurred while in combat may be more difficult because the VA is not required to accept the veteran’s statement as fact. However, the VA is required to weigh and consider the veteran’s statement when making this important determination.
According to the U.S. Court of Appeals for Veterans Claims, the veteran does not have to provide evidence corroborating his or her statement. However, corroborating evidence would certainly be helpful in persuading the VA to accept the veteran’s statement that he or she was engaged in combat.
h3 id=”h-ways-to-corroborate-a-veteran-s-statement-about-their-combat-service”>Ways to Corroborate a Veteran’s Statement about Their Combat Service
- The veteran’s combat service may be indicated on service records. This can include documentation of any combat decoration, citation, or reward.
- Any evidence that shows that the area or base the veteran was in was attacked by the enemy.
- Whether the veteran in question was directly exposed to fire does not matter.
- Any documentation that the veteran received hazardous duty pay
- “Buddy statements” from fellow soldiers regarding the veteran’s inclusion in combat
h3 id=”h-step-by-step-application-of-how-a-veteran-s-statement-is-analyzed”>Step by Step Application of How a Veteran’s Statement Is Analyzed
The next step after establishing you are a combat veteran in the VA claims process is for the VA to evaluate your statements and make sure that you meet certain conditions. If these conditions are met, the combat veteran’s lay statements regarding the injury or disease will be accepted.
To examine your statements the VA claims process will undergo three steps.
STEP 1: The Combat Veteran’s Evidence Must Be Satisfactory
The VA will first focus on the evidence that has been provided by the combat veteran to determine whether it is “satisfactory.” There are three sub-steps involved in making this decision:
STEP 1A: What evidence does the “satisfactory” requirement apply to?
- In this case, the “satisfactory” requirement applies only to evidence submitted by the veteran. This could include: statements, any testimony you make, and any documents you present.
STEP 1B: What does “satisfactory” evidence mean?
- According to the U.S. Court of Appeals for Veteran Claims, “satisfactory” means credible, plausible, or capable of being believed.
STEP 1C: How do you determine whether evidence is “satisfactory?”
- Where testimony is provided in person, the VA may consider behavior and expressions, plausibility of the testimony, and whether the testimony is consistent with other evidence.
- Where the evidence is a written document, the VA may consider the consistency of that document, plausibility of that document, and consistency of that document when compared to other evidence. In any situation where the evidence is equal on both sides, the veteran will get the benefit of the doubt.
Step 2: The Evidence Provided by the Combat Veteran Must Be Consistent with Circumstances of Service
The U.S. Court of Appeals for Veterans Claims has established certain principles for determining whether a combat veteran’s lay evidence is consistent with the circumstances of service.
The principles are as follows:
- A combat veteran’s medical records should not be used to determine whether the veteran’s statements are consistent with his or her circumstances of service. The only exception to this is when the veteran’s medical records show specific inconsistencies.
- ·In circumstances where there is equal evidence on both sides, the veteran will receive the benefit of the doubt.
Step 3: There Cannot Be Clear and Convincing Evidence in the Record against Incurrence or Aggravation during Combat
Once Step 1 and Step 2 are satisfied, the next step in the VA claims process is to look at any negative evidence that might prove the veteran’s statements to be false. If there is no unfavorable evidence, the VA will accept the combat veteran’s statement.
However, you should note that even if there is negative evidence, it is still difficult for the VA to oppose a combat veteran’s statement. That is because the VA claims process requires the high standard of “clear and convincing” negative evidence to be presented, as opposed to just a “fair preponderance of evidence.”
Chapter 16: Agent Orange Exposure
h3 id=”h-benefits-available-to-veterans-exposed-to-agent-orange”>Benefits Available to Veterans Exposed to Agent Orange
Chemical herbicides such as Agent Orange were used during the Vietnam Era to defoliate areas of Vietnam and in some cases, it was used near the Demilitarized Zone (DMZ) in Korea. Herbicides were also used to provide perimeter base control on bases in Vietnam and Thailand, along the Ho Chi Min Trail and near the Demilitarized Zone in Korea beginning in September of 1967. Herbicides were tested at a variety of locations prior to being used in Vietnam. In addition, herbicides were stored at various locations such as Johnston Island, Guam, and Gulfport, Mississippi, during various time periods.
Exposure to herbicides, including Agent Orange, has been associated with a variety of cancers and other diseases.
- A veteran with disabilities associated with herbicide exposure, may qualify for health care, vocational rehabilitation and payment of monetary compensation benefits.
- A surviving spouse or surviving child of a veteran exposed to herbicides may be eligible for benefits including Dependency and Indemnity Compensation (DIC) benefits, CHAMP-VA healthcare and educational benefits.
- Veterans who served on “brown” water are eligible for a presumption of service connection for any disability recognized as associated with exposure to herbicides even if they did not have “boots on the ground.”
h3 id=”h-qualifying-for-va-benefits-after-herbicide-exposure”>Qualifying for VA Benefits after Herbicide Exposure
In order to qualify for service connection based upon herbicide exposure, veterans must establish that they have a current disability related to exposure to herbicides during military service. Once a current disability is established by medical evidence, it is necessary to determine where the veteran was located during military service and whether such location(s) involved exposure to herbicides.
The critical questions are:
- Where was the veteran?
- When was the veteran there?
- Where were the herbicides?
- When were the herbicides there?
Records of herbicide use were not maintained so finding documentation can be difficult, but the VA continues to identify information and evidence concerning locations of exposure.
h3 id=”h-veterans-outside-of-vietnam-eligible-for-va-benefits-based-on-herbicide-exposure”>Veterans Outside of Vietnam Eligible for VA Benefits Based on Herbicide Exposure
If a veteran can establish that he or she was exposed to herbicides on a direct basis, VA will apply the presumption of nexus granted to diseases associated with herbicide exposure.
Of course, Veterans who served during active military, naval, or air service in the Republic of Vietnam during the period beginning January 9, 1962 and ending May 7, 1975 may qualify for a presumption of exposure to herbicide agents. The Republic of Vietnam includes the land mass of Vietnam and its inland waterways.
h3 id=”h-proving-exposure”>Proving Exposure
Regardless of location, establishing evidence that a veteran had exposure is the first hurdle to acquiring benefits. Evidence of “boots on the ground” might include:
- a veteran’s military records,
- service treatment records (STR),
- deck logs and/or
- ship newsletters, cruise books, buddy statements or photographs.
h3 id=”h-proving-you-are-a-brown-water-naval-veteran”>Proving You Are a Brown Water Naval Veteran
Vietnam naval veterans who operated in brown (shallow) waters may qualify for service connection due to herbicide exposure. In order to prove exposure as a naval veteran, you must:
- Provide documentation of your location during relevant military service;
- identify your ship; and
- obtain evidence of the ship’s location in Vietnam waters
To qualify for benefits, veterans should provide documentation, which may include one or many of the following sources:
- a veteran’s copies of the ship logs or command history;
- documentation on an official military site concerning the ship on which he or she served during the relevant time frame;
- the veteran’s “201” military service file, which VA or the veteran should request from the National Personnel Records Center;
- a “PIES” request to VA staff at the National Personnel Records Center;
- documentation on the C and P Web site;
- the Dictionary of American Fighting Ship Index on the Navy history site (www.history.navy.mil/danfs/index.html);
- National Archive “CONGA;”
- deck logs from the Joint Services Records Research Center (JSRRC); and/or
- documents such as cruise books and photographs found on the Internet at individual ship and organization sites
h3 id=”h-new-diseases-added-to-va-agent-orange-presumptive-illnesses-list”>New Diseases Added to VA Agent Orange Presumptive Illnesses List
The Department of Veterans Affairs (VA) has added Parkinson’s disease and ischemic heart disease to the list of “presumptive illnesses” related to Agent Orange exposure. In addition, VA expanded the presumption for chronic lymphocytic leukemia to include all chronic B-cell leukemias, such as hairy cell leukemia. These conditions are presumed to be service-connected to herbicide exposure in Vietnam.
Vietnam Veterans with these illnesses are able to claim VA disability benefits and health care services without having to prove that their conditions are connected to Agent Orange exposure. The new policy took effect in late 2010 and applies to Veterans who served in Vietnam anytime during the period beginning January 9, 1962, and ending on May 7, 1975. It does not apply to Veterans who only served on “Blue Water” Navy ships in the region.
The VA’s decision to include these conditions brings the total number of categories of presumed illnesses linked to Agent Orange to 14.
The VA already presumes that the following conditions are Agent Orange related:
| Adult Fibrosarcoma AL Amyloidosis (also known as Primary Amyloidosis) Alveolar Soft Part Sarcoma Angiosarcoma B-cell Leukemias Birth Defects Cancer of the Bronchus Cancer of the Larynx Cancer of the Lung Cancer of the Prostate Cancer of the Trachea Chloracne Chronic Lymphocytic Leukemia Clear Cell Sarcoma of Aponeuroses Clear Cell Sarcoma of Tendons Congenital Fibrosarcoma Dermatofibrosarcoma Ectomesenchymoma Epithelioid Malignant Leiomyosarcoma Epithelioid Malignant Schwannoma Epithelioid Sarcoma Extraskeletal Ewing’s Sarcoma Hairy-cell Leukemia Hemangiosarcoma Hodgkin’s Disease Infantile Fibrosarcoma |
Ischemic Heart Disease Leiomyosarcoma Liposarcoma Lymphangiosarcoma Lymphoma Malignant Fibrous Histiocytoma Malignant Giant Cell Tumor of the Tendon Sheath Malignant Glandular Schwannoma Malignant Glomus Tumor Malignant Hemangiopericytoma Malignant Mesenchymoma Malignant Schwannoma with Rhabdomyoblastic Multiple Myeloma Non-Hodgkin’s Lymphoma Parkinson’s Disease Peripheral Neuropathy Porphyria Cutanea Tarda Proliferating (systematic) Angiendothelimatosis Rhabdomyosarcoma Sarcoma Soft Tissue Sarcoma Spina Bifida Subacute Peripheral Neuropathy Synovial Sarcoma Type 2 Diabetes (also known as Diabetes Mellitus) |
Recent Studies Regarding Possible Updates to Agent Orange-related Diseases
Recommendations have been made to the VA by the Institute of Medicine (IOM) regarding recent information about Agent Orange related diseases. The U.S. Department of Veterans Affairs is not bound by OIA committee’s recommendations. At the time of this writing, VA is reviewing these findings, and has yet to take action towards implementing any of them.
- The IOM states a link could exist between AO exposure and
- Bladder cancer
- Hypothyrodidism
- A “reversal” was made by IOM for spina bifida in children of Vietnam vets. This disease is downgraded by IOM from “limited or suggestive” category to “inadequate or insufficient” category.
- Institute of Medicine also clarified changes in how the VA evaluates claims for conditions with Parkinson’s-like symptoms.OIA states that Vets with Parkinson’s-like symptoms – but without a formal diagnosis of Parkinson disease – should be considered eligible under the presumption that Parkinson’s disease and the veterans’ service are connected. To exclude a claim for a condition with Parkinson’s-like symptoms, the onus would fall to the VA to “establish the role of a recognized factor other than the herbicides sprayed in Vietnam” on a case-by-case basis.
- The VA has not found hypertension or stroke to be presumptively related to herbicide exposure in Vietnam, but the IOM committee reaffirmed their previous findings that put both conditions in the limited or suggestive evidence of association category.
h3 id=”h-benefits-for-surviving-family-of-veterans-exposed-to-agent-orange”>Benefits for Surviving Family of Veterans Exposed to Agent Orange
Surviving spouses, dependent children and dependent parents of Veterans who were exposed to Agent Orange and died as the result of diseases related to Agent Orange exposure may be eligible for a monthly payment called Dependency and Indemnity Compensation (DIC).
See Benefits for Surviving Family of Veterans Exposed to Agent Orange.
h3 id=”h-effective-dates-for-agent-orange-exposure-in-vietnam”>Effective Dates for Agent Orange Exposure in Vietnam
Many Vietnam veterans and their survivors are eligible to have VA compensation claims for disability or death benefits granted as a result of their exposure to Agent Orange (AO). Some of these veterans qualify for a special set of effective date rules that are significantly more favorable to them than the normal effective date rules. This is a result of the Nehmer v. U.S. Veterans Association class action regulation which, among other things, made three new diseases eligible for service connection due to AO exposure. These diseases are Parkinson’s disease, ischemic heart disease, and chronic B-cell leukemias (including hairy cell leukemia).
Because of the Nehmer order, the VA has been forced to go back and re-decide over 147,000 VA compensation claims that were filed between September 25, 1985, and August 31, 2010. If it is decided that disability and death benefits are to be awarded to any of these claimants, the VA will have to retroactively pay them these benefits based on the new, extremely favorable effective date rules. This could lead to over $1 billion in retroactive payments to Vietnam veterans and their survivors.
The National Veterans Legal Services Program (NVLSP) has set up a Nehmer Lawsuit Division to help make sure that the VA provides qualified veterans and their surviving families with the proper compensation. If you or your disability denial attorney contacts them, they will answer any questions you may have.
h3 id=”h-qualifying-diseases-and-their-special-effective-dates-for-agent-orange-va-compensation-claims”>Qualifying Diseases and Their Special Effective Dates for Agent Orange VA Compensation Claims
There are many different Agent Orange-connected diseases that a Vietnam veteran may have been afflicted with. Each of these diseases has been assigned a corresponding effective date that is used to determine the amount of retroactive benefits that they or their surviving family members are entitled to when making VA compensation claims.
The following is a list of these diseases and their effective dates as listed in the Nehmer Training Guide, Appendix 1 – List of Presumptive Conditions in 38 C.F.R. § 3.816:
- Chloracne – 2/6/91
- Soft-tissue sarcoma (STS) – 9/25/85
- Non-Hodgkin’s lymphoma – 8/5/64
- Porphyria cutanea tarda – 2/3/94
- Hodgkin’s disease – 2/3/94
- Cancer of the lung – 6/9/94
- Cancer of the larynx – 6/9/94
- Cancer of the bronchus – 6/9/94
- Cancer of the trachea – 6/9/94
- Multiple myeloma – 6/9/94
- Prostate cancer – 11/7/96
- Acute and subacute peripheral neuropathy – 11/7/96
- Type 2 Diabetes – 5/8/01
- Chronic lymphocyte leukemia – 10/16/03
- Primary AL Amyloidosis – 5/7/09
- Ischemic heart disease – 8/31/10
- Chronic B-bell Leukemias (except chronic lymphocytic leukemia) 8/31/10
- Parkinson’s disease – 8/31/10
A Veteran can cite the “Nehmer Training Guide” when trying to get the VA Regional Office to assign the correct effective date for VA compensation claims for any of these Agent Orange-related diseases.
h3 id=”h-why-agent-orange-effective-date-rules-for-death-and-disability-claims-were-established”>Why Agent Orange Effective Date Rules for Death and Disability Claims Were Established
The Nehmer order forced the VA to acknowledge that there were many other serious diseases that could be caused by AO exposure. Now, any Vietnam veteran who is afflicted with any of these many AO-related diseases is eligible for a service connection for that disease. This even applies to veterans and their surviving family members who have been denied benefits for the same disease in the past.
One of the most important things the Nehmer lawsuit established was the new effective date rules, which are very favorable to veterans and their families. However, even after these new dates were approved, the VA did not make them public.
In fact, they even went out of their way to hide and purposely misinterpret these rules in order to pay out less money to claimants and their families. Because of this, it took almost a decade for the veterans, their surviving family members, and any VA disability attorney they may have hired to learn exactly what the new dates were and what they really meant.
h3 id=”h-the-national-veterans-legal-services-program-and-ao-exposure-disability-claims”>The National Veterans Legal Services Program and AO Exposure Disability Claims
For years, the VA continued to do all it could to deny and underpay death and disability claims related to Agent Orange exposure. Time and time again, lawyers from the National Veterans Legal Services Program (NVLSP) repeatedly took the VA to court and forced them to pay huge sums of retroactive benefits in order to make things right. The NVLSP is available to answers questions or provide assistance on all matters related to AO exposure disability claims.
h3 id=”h-what-communications-count-as-disability-claims-for-agent-orange-related-diseases”>What Communications Count as Disability Claims for Agent Orange-Related Diseases?
Any disability claims for Agent Orange-related diseases that were denied or filed after September 24, 1985, and before the List of Presumptive Condtions was published, could be considered Category 1 claims. In these cases, the rules that define what is considered to be an official disability compensation claim are very liberal.
Some examples of communications that should be sufficient to allow a veteran to qualify for the special Agent Orange effective date rules for disability compensation are:
- An official VA document submitted by the veteran to the VA stating that the veteran should be granted service-connected disability benefits for a specific disease that is listed in the List of Presumptive Condtions. It is not necessary that this document refers specifically to Vietnam or Agent Orange.
- Disability claims made by a veteran for a disease that was never specifically identified. However, while the claim is pending, medical records that diagnosed the veteran with a Table 8-1 disease is filed with the VA.
- A compensation claim a veteran files for a disability that is not listed in the List of Presumptive Condtions, but while the claim was pending, the veteran was officially diagnosed with a listed disease that is put into their VA claim file. This rule is often violated by the VA when setting effective dates. In order to improve compliance with this rule, the VA added more details to its Nehmer training guide.
h3 id=”h-do-medical-records-count-as-disability-claims”>Do Medical Records Count as Disability Claims?
A veteran’s medical records do not count as a claim by themselves. However, if medical records are present at the time the veteran files separate disability claims, the condition shown on the medical records will be considered part of those claims.
h3 id=”h-other-requirements-that-exist-for-agent-orange-va-claims”>Other Requirements That Exist for Agent Orange VA Claims
In order for a Vietnam veteran to fit into Category 1 with regards to Agent Orange-related diseases, you must have either filed the VA claims or had them denied during a specific period of time. This period runs from September 24, 1985, to whatever date the ruling on the disease you suffer from was made official. This publication date can be found in the second column of the Nehmer Training Guide, Appendix 1 – List of Presumptive Conditions in 38 C.F.R. § 3.816.
h3 id=”h-category-1-rules-for-agent-orange-va-claims”>Category 1 Rules for Agent Orange VA Claims
The Category 1 rules are very clear and easy to understand when it comes to disability claims that were filed during the window period. These will always qualify a veteran for Category 1 status.
The rules can be a bit more confusing when trying to figure out if VA claims that were denied during the window period will still qualify the sufferer for Category 1. Some of these rules are:
- If a veteran had his or her disability claim for an AO-related disease denied before September 24, 1985, but filed a timely appeal and ultimately received a final denial after said date, he or she would be included in Category 1.
- If a veteran had an AO-related disability claim denied before September 25, 1985, and the final denial came after said date, he or she would not be included in Category 1. This is because the time period for a veteran to file a notice of disagreement or appeal expired after said date.
- If a veteran filed more VA claims for an already-denied disability after September 25, 1985, these new claims would qualify the veteran for Category 1.
h3 id=”h-effective-date-rule-for-veterans-who-filed-category-1-va-claims”>Effective Date Rule for Veterans Who Filed Category 1 VA Claims
Vietnam veterans who file VA claims that qualify them for Category 1 will normally be given extremely favorable effective dates for their service-connected claims. In most cases, the effective dates for these disability claims will be the actual date on which the VA first received the claim. However, there are two exceptions to this rule:
- If there is no evidence to show that the disease in question was at least disabling to the degree of 10 percent on the date the VA received the claim, then the effective date will be the date the disease became disabling to a degree of at least 10 percent.
- If the Category 1 disability claims were filed with the VA within one year of the veteran’s discharge from service, the effective date will be the day after the date of discharge.
h3 id=”h-what-if-the-veteran-filed-multiple-va-claims-that-fit-within-category-1″>What If the Veteran Filed Multiple VA Claims that Fit within Category 1?
In many situations, a Vietnam veteran might file more than one claim that fits within Category
1. If this is the case, the effective date is determined using the date of the first claim that was filed within the Category 1 window period.
For example, if a Vietnam veteran filed a disability claim for a disease in 1993 and was denied, then filed VA claims for the same disease again in 1996 after the disease was added to the List of Presumptive Conditions, the effective date would be set at the 1993 date on which they first filed the claim.
h3 id=”h-effective-date-rules-for-category-2″>Effective Date Rules for Category 2
The effective date rules for Category 2 VA claims determine whether a Vietnam veteran’s surviving family members will qualify for death compensation or death pension.
These rules apply to the families of veterans who served overseas in Vietnam and died from a disease that was at least caused in part by one of the Agent Orange-related diseases on the List of Presumptive Conditions.
In order for a surviving family member to be included in Category 2, the claim in question must meet the following criteria:
- There must have been a death benefits claim for either DIC or death pension. A VA disability attorney should note that a claim for pension is automatically considered as a claim for DIC even if the survivor indicated that the veteran’s death was not due to service.
- The VA claims in question must have been denied or filed in the effective date window, which is after September 24, 1985, and before the publication date in the List of Presumptive Conditions for the disease that led to the veteran’s death.
Once it is decided that a DIC claim fits within Category 2, the effective date is the next thing that needs to be determined. This effective date is normally set on the date the VA received the claim for DIC or death pension.
It can also be set on the first day of the month in which the veteran’s death occurred in cases where the claim was filed within one year of the veteran’s death.
h3 id=”h-do-va-claims-for-service-connected-burial-benefits-count-as-dic-claims”>Do VA Claims for Service-Connected Burial Benefits Count as DIC Claims?
In certain cases, claims for service-connected burial benefits will also count as DIC claims for the purpose of qualifying a surviving family member for Category 2 status. For example:
- A veteran’s surviving spouse filed an application for burial benefits and indicated on the form that the cause of death was due to service. This caused the VA to forward a DIC claim application to the spouse, who filled it out and returned it to the VA within one year.
- A veteran’s surviving spouse filed an application for burial benefits and indicated on the form that the cause of death was due to service. The VA did not forward a DIC claim application to the spouse. Due to the VA’s failure to provide the correct VA claims application to the spouse, the one-year filing period for the DIC application never began; therefore, DIC must be retroactive to the date of the application for burial benefits.
Chapter 17: Persian Gulf Veterans’ Claims
As with other claims, the disability claims process for veterans of the Persian Gulf War can be confusing. However, the road to gaining your rightfully deserved compensation may be less treacherous than you think.
Several cases decided by the US Court of Appeals for Veterans Claims have made it easier for veterans to receive their disability benefits by way of the presumptive service connection.
h3 id=”h-how-presumptive-service-connection-affects-disability-claims”>How Presumptive Service Connection Affects Disability Claims
In order to be eligible for benefits, a veteran must prove that he or she is suffering from a “qualifying chronic disability” that was incurred during active military service.
In 1994, Congress made it easier for veterans who specifically served in the Persian Gulf War, including both Operations Desert Shield and Desert Storm, to prove a service connection by enacting 38 USC Section 1117 and 38 USC Section 1118.
The aforementioned sections of the US Code establish a “presumptive” connection between the veteran’s qualifying disability and the veteran’s military service. Previously, the vague nature of many of the multi-symptom ailments affecting Gulf War vets had made both verifiable diagnoses and proven connection to military service almost impossible to attain, leading to many cases of veterans being denied their rightful benefits.
Under Section 1117, you merely have to prove that your qualifying disability manifested during service in the Persian Gulf or to a degree of 10 percent after being discharged from active duty. This altered rule makes it much easier for Gulf War vets to receive their benefits.
h3 id=”h-how-section-1117-affects-other-veterans-disability-claims”>How Section 1117 Affects Other Veterans’ Disability Claims
The limits of Section 1117 extend the presumptive service connection to military veterans who served in the Persian Gulf area even after the conclusions of Operations Desert Shield and Desert Storm. Thus, all veterans of Operation Iraqi Freedom and Operation Enduring Freedom, as well as all active military serving in the Gulf area, can make use of the expedited VA claims process made possible by Section 1117.
However, although Congress enacted this US Code section to protect the heroic men and women who served and continue to serve our country, the VA still has ways of denying benefits to deserving veterans.
The VA may try to prove that your qualifying disability was not caused by the stresses of active service but by outside events before or after service, or even by willful misuse of alcohol or drugs.
h3 id=”h-three-requirements-for-establishing-a-presumptive-connection-when-making-disability-claims”>Three Requirements for Establishing a Presumptive Connection When Making Disability Claims
The first requirement that must be fulfilled in order to receive the presumptive service connection is definitely the simplest – you must prove that you were on active duty somewhere in the Southwest Asian Theater sometime on or after August 2, 1990.
Active duty includes time on land or in sea or air, and most countries surrounding the Persian Gulf as well as Afghanistan are included. The official language from the Veterans Benefits Manual covers “Iraq, Kuwait, Saudi Arabia, the neutral zone between Iraq and Saudi Arabia, Bahrain, Qatar, the United Arab Emirates, Oman, the Gulf of Aden, the Gulf of Oman, the Persian Gulf, the Arabian Sea, the Red Sea, and the airspace above these locations.”
The second requirement deals with proving that you have a “qualifying chronic disability.” Simply put, you must be suffering from some sort of undiagnosed illness, a medically unexplained chronic multi-symptom illness, or any diagnosed illness previously ruled eligible.
A qualified disability lawyer can help you parse which of your symptoms makes you eligible and which do not.
Finally, you will need to prove that your disability manifested during the eligible time period. Your symptoms must have manifested either during active service in the Persian Gulf or “to a degree of 10 percent or more during the presumptive period” that follows active duty.
The length of the presumptive period varies depending on the nature of the illness or ailment.
h3 id=”h-are-there-special-considerations-for-the-disability-claims-of-certain-veterans”>Are There Special Considerations for the Disability Claims of Certain Veterans?
The VA recognizes that veterans who served in Iraq or Afghanistan during Operation Iraqi Freedom or Operation Enduring Freedom are entitled to some special considerations when it comes to their disability claims. A few injuries and ailments common among veterans of Iraq and Afghanistan have been made eligible to establish the presumptive service connection that is required to receive benefits.
Studies have shown that incidences of traumatic brain injury, or TBI, are much higher when it comes to veterans of these two conflicts. In fact, TBI is so prevalent that is often considered to be the “signature disability” of vets returning from Iraq and Afghanistan.
In addition, the VA has acknowledged that several environmental hazards present in Iraq, Afghanistan, and Djibouti have led to an increased risk for certain other ailments. The VA and has implemented special considerations to deal with victims of these hazards.
h3 id=”h-tbi-signs-and-symptoms-that-are-relevant-to-veteran-disability-claims”>TBI Signs and Symptoms That Are Relevant to Veteran Disability Claims
Veterans who served in Operation Iraqi Freedom or Operation Enduring Freedom were at a unique risk to injury from enemy combatant IED blasts. At least one of the symptoms must have manifested immediately after the event for a successful diagnosis of TBI.
Some of the symptoms that indicate a brain injury include:
- Loss of or lessened consciousness
- Loss of memory
- Confusion, disorientation, or other evidence of altered mental state
- Neurological deficits such as loss of balance, praxis, aphasia, sensory loss, or paresis/plegia
- Intracranial lesion
h3 id=”h-environmental-hazards-that-are-relevant-to-veterans-disability-claims”>Environmental Hazards That Are Relevant to Veterans Disability Claims
Several environmental hazards present in Iraq, Afghanistan, and Djibouti are known to have contributed to an increase in veterans’ health issues.
Burn pits that released toxic substances were utilized by the US military to dispose of waste starting in 2001.
Dust storms, local industry emissions, and a few specific incidents, such as the three-week burning of the Mishraq Sulfur Mine in 2003, are also noted as having increased veterans’ exposure to dangerous environmental hazards.
A wide range of respiratory, neurological, autoimmune, cardiopulmonary, and skin disorders have been linked to time served in the area of these environmental hazards.
If you are an Operation Iraqi Freedom or Operation Enduring Freedom veteran and you feel that you may have been affected by the factors listed under these special considerations, think about hiring a qualified disability attorney to help you fight for the veterans benefits that you deserve.
Chapter 18: Upgrading a Veteran’s Discharge Status
h3 id=”h-can-upgrading-a-discharge-make-you-eligible-for-veterans-benefits”>Can Upgrading a Discharge Make You Eligible for Veterans Benefits?
If you were the recipient of a less than honorable military discharge, then you already know that you are ineligible for veterans benefits. But by upgrading your discharge, you can start receiving the compensation that you are entitled to as a former member of the US armed forces.
All branches of the service have two separate discharge upgrading forums: a Discharge Review Board (DRB) and a Board for Correction of Military Records (BCMR) for your branch of the armed services. Once the discharge has been changed from less than honorable to general or honorable in one of these two forums, the VA Board must then be utilized to grant veterans benefits.
In general, only veterans who received an honorable discharge or general discharge can be considered eligible for benefits. If you feel that you were issued an incorrect discharge –other than honorable, bad conduct, or dishonorable – you can fight to overturn that judgment and receive the benefits that you deserve.
With the help of a qualified attorney and veterans’ advocate, you might also be able to change your bad discharge to a disability separation or simply a retirement. Although you will not receive damages for an incorrectly characterized discharge, you may be eligible to receive back pay benefits if your discharge is deemed illegal or wrongful.
h3 id=”h-risks-associated-with-upgrading-a-discharge-to-receive-veterans-benefits”>Risks Associated With Upgrading a Discharge to Receive Veterans Benefits
Many veterans worry that fighting a discharge can lead to stigmatization or even potential harassment. However, the discharge upgrading process is completely confidential to all individuals and organizations outside the military.
We will add that it is true that members of the VA Board may not be incredibly sympathetic to veterans with less than honorable discharges.
That is why it is so incredibly helpful to have the assistance of a qualified veterans advocate as you navigate your way through the VA claims process.
h3 id=”h-is-it-easier-to-become-eligible-for-veterans-benefits-through-discharge-upgrading-or-va-adjudication”>Is It Easier to Become Eligible for Veterans Benefits Through Discharge Upgrading or VA Adjudication?
There are several different avenues available to those who wish to upgrade their discharges in order to become eligible for veterans benefits. The circumstances of your discharge will determine which path is right for you.
If you are unsure as to which process will be most effective in gaining your benefits, consult VA accredited attorney who can help you make the right choice.
All branches of the armed service offer the Discharge Review Board (DRB) and the Board for Correction of Military Records (BCMR) in order for veterans to upgrade their discharges. VA adjudication provides another avenue through which servicemen and women can obtain veterans benefits, though the VA does not have the power to upgrade a discharge.
h3 id=”h-choosing-the-right-path-to-be-eligible-for-veterans-benefits”>Choosing the Right Path to Be Eligible for Veterans Benefits
There are a series of factors that must be taken into consideration when choosing whether discharge upgrading or VA adjudication is the best fit for your situation. When it comes to discharge upgrading, the choice between filing with the DRB or BCMR can be affected by each forum’s statute of limitations.
Veterans have a hard and fast 15 years from the date of discharge to file with the DRB – and this forum makes no exceptions or waivers. On the other hand, BCMR only has a three-year statute of limitations from the date of discovery of the discharge error, but that forum can usually waive this limit on request.
You must also take into account each forum’s eligibility rules concerning the classification of your discharge. Veterans with certain statutory bars can only file with the BCMR.
Similarly, veterans with bad conduct discharges or dishonorable discharges issued by general court-martials can only file with the BCMR.
If you are not encumbered by a statutory restriction or a certain classification of discharge and you have a compelling personal story, applying to the DRB may be the best strategy. This is because the DRB review process guarantees a personal hearing, which means you will have the chance to make your case in person.
Most veterans apply for a discharge upgrade with the DRB or the BCMR and then apply for veterans benefits eligibility with the VA Board only after receiving the upgrade. But it is possible to skip straight to VA adjudication. The VA Board is much more likely to grant eligibility to veterans who have upgraded their discharges than to veterans who still carry any discharge other than honorable.
There are a few rare cases in which it may be advantageous to apply simultaneously to a discharge review forum and to the VA Board, or even to the VA Board before the forum, but the problem of getting military records to multiple agencies at the same time is usually too much of an obstacle.
h3 id=”h-becoming-eligible-for-veterans-benefits-through-discharge-review”>Becoming Eligible for Veterans Benefits through Discharge Review
If you have a less than honorable discharge preventing you from receiving veterans benefits and you feel that it was issued unfairly, you may be able to upgrade your discharge and become eligible for compensation.
The discharge review process is fairly straightforward, although it helps to have a qualified veterans advocate assist you in presenting your case.
Any veteran may at any time apply to have his or her discharge reviewed. You’ll have to go through either the Discharge Review Board (DRB) or the Board of Correction of Military Records (BCMR). There are several considerations to weigh when choosing between the DRB and the BCMR:
- If your discharge is less than 15 years old and is a general discharge other than honorable discharge, uncharacterized discharge, or bad conduct discharge from a special court-martial, go with the DRB and use a DD Form 293.
- If your discharge is more than 15 years old OR is a bad conduct or dishonorable discharge from a general court-martial, apply to the BCMR with a DD Form 149.
Once you’ve chosen the forum to which you want to apply, you will need to request a copy of your military records using an SF 180 form. It is usually best not to file your claim until you have received the copy of your records.
After filing, the review process may take anywhere from six to 12 months. Occasionally, it takes longer. If your discharge upgrade is successful, you’ll then need to begin the VA claims process to start receiving the veterans benefits that you’ve earned.
h3 id=”h-what-factors-will-make-a-discharge-review-more-likely-to-result-in-veterans-benefits-eligibility”>What Factors Will Make a Discharge Review More Likely to Result in Veterans Benefits Eligibility?
Unfortunately, the burden is on the veteran to prove that the facts presented by military records do not tell the whole story.
Introducing and developing evidence to counter or give more detail to the facts found in your records will be crucial to building a successful argument and winning your veterans benefits. You and your lawyer will want to discuss the specific strategy you will use to make the best possible discharge review case.
The review boards do tend to reconsider the discharge decision under current standards. If your discharge was based on factors that would today make such a discharge illegal, such as homosexuality, alcoholism, personality disorders without a psychiatric diagnosis, “unsuitability,” or even bed-wetting, it may be fairly easy to get your discharge upgraded.
In cases where the discharge basis was not so blatantly illegal, you and your lawyer will need to develop a defense that proves your good character.
Evidence of your education and work achievements, community service history, letters of recommendation, or any documents that support your good character will go a long way in proving to the review board that you deserve to have your discharge upgraded.
Chapter 19: Get Help from an Accredited VA Attorney, Claims Agent or Representative
Filing a claim for veterans disability benefits should be a straightforward task that is met with respect and processed with urgency. Yet for the thousands of veterans in dire need of disability compensation, the process is burdened by unforgivable delays and denials.
A veteran may wait 4 months to 2 years to receive a decision of benefits. If the claim is denied, a disabled vet can spend years more fighting and waiting for benefits. The road to winning VA compensation claims cases can be immensely improved with the help of a qualified representative.
h3 id=”h-who-can-assist-a-veteran-with-a-va-claim-for-benefits”>Who Can Assist a Veteran with a VA Claim for Benefits?
Federal law states that the only individuals with the authority to assist a veteran in the preparation, presentation, and prosecution of a claim for VA benefits are those who are accredited by VA as an attorney, agent, or representative of a VA-recognized veterans service organization.
“Accredited by the VA” means a person has gone through the VA’s official training process and is recognized by the U.S. Department of Veterans Affairs as being capable of assisting claimants with their affairs before VA. Accreditation is required to ensure disabled veterans who seek help are receiving efficient and competent representation. The VA lawyer or agent must also comply with the power-of-attorney requirements and the fee agreement requirements as set forth by law.
The VA allows only one exception to the accreditation rule: any one person can help any veteran – one-time only – with a claim. To help any veteran a second time requires accreditation.
The forms appointing the accredited representative will be filed with the VA office that has jurisdiction over your claim (generally a VA Regional Office or the Board of Veterans’ Appeals).
h3 id=”h-how-can-i-find-an-accredited-va-attorney-agent-or-representative”>How Can I Find an Accredited VA Attorney, Agent or Representative?
The VA provides a searchable list of accredited VA attorneys, Claims Agents or Veterans Service Organizations (VS) Representatives here:
h3 id=”h-when-can-the-accredited-attorney-or-agent-charge-fees-for-service”>When Can the Accredited Attorney or Agent Charge Fees for Service?
According to federal law, no person or organization may charge a fee for helping the veteran prepare his or her application for VA benefits or presenting the claim to VA.
A VA-accredited lawyer or agent is allowed to charge fees for assistance on a claim only after VA has issued a decision on a claim and (having disagreed with the decision) the veteran has filed a Notice of Disagreement to begin the appeal of that decision.
There is some history behind this policy. For decades following the Civil War, federal policy was generally against the idea of veterans having legal representation in claims against the VA. Over the years, Congress began to remove some of the restrictions against legal counsel.
Not long ago, legislation was passed with the Veterans Benefits, Health Care, and Information Technology Act of 2006. This act permits a lawyer to charge a reasonable fee for representation after a Notice of Disagreement (NOD) has been filed—so long as the NOD was filed on or after June 20, 2007.
The VA reviews fees for reasonableness. The VA has ruled that any fee of more than one-third of past due benefits will be considered unreasonable. This change in how veterans are able to seek qualified attorneys has dramatically increased the success rate of disability claims.
h3 id=”h-secure-your-va-disability-benefits-through-an-accredited-veterans-claim-attorney-agent-or-representative”>Secure Your VA Disability Benefits through an Accredited Veterans Claim Attorney, Agent or Representative
The VA faces immense challenges. It is hard pressed to improve its services to veterans, specifically to speed up the process of decisions and appeals, end the backlog of claims, and perfect the accuracy and consistency of decisions.
After dealing with the VA for a while, many veterans realize that despite the VA’s responsibility to assist veterans with their claims, there are many ways that the VA can get around or even blatantly ignore its responsibilities.
The right representative can be especially helpful when it comes to obtaining doctor’s statements that are detailed enough for the VA to decide in your favor. A qualified advocate will be able to evaluate all medical evidence to ensure it meets the level of detail required by the VA.
The rules and restrictions that affect VA claims are notoriously difficult to interpret and understand. If you’re even slightly unsure of the process for proving the many requirements touched upon in this guide, a veterans’ advocate or lawyer can clarify everything that you need to know, and take the burden off of your shoulders. Call Marc Whitehead & Associates today at 800-562-9830.
Further reading:
Visit the U.S. Department of Veterans Affairs website at https://www.va.gov/
U.S, Department of Veterans Affairs Disability Compensation Information: https://www.benefits.va.gov/benefits/
U.S, Department of Veterans Affairs Pension Information: https://www.benefits.va.gov/pension/
References
- U.S. Department of Veterans Affairs website. Accessed January 1, 2016. www.va.gov
- Title 38 Code of Federal Regulations. Accessed January 1, 2016. https://www.benefits.va.gov/warms/topic-title38.asp; including 38 C.F.R. § 3.304; 38 C.F.R. § 3.816; 38 C.F.R. § 14.627(a); 38 CFR§ 14.630; 38 C.F.R. § 14.631; 38 C.F.R. § 14.636(c); 38 C.F.R. § 14.636(g);
- U.S. Code: Title 38 – Veterans Benefits; Title 38 USC § 5903 and Title 38 USC § 5904(c) (1).
- Marc Whitehead, Strategies for a Winning Campaign: Veterans Disability Claims. 2010. Accessed January 1, 2016. /veterans-disability-claims-ebook
- Marc Whitehead & Associates, Attorneys at Law, LLP. A National Disability Claims Law Firm. Accessed January 1, 2016. https://disabilitydenials.com/.
Back to disabilitydenials.com




